53 The Health Impacts of Toxic Metals
Intro-
Toxic metals, often called heavy metals, are metals and metal compounds that negatively affect human health, especially in large amounts. While small amounts of certain metals are essential for life, excessive exposure can lead to toxicity as they accumulate in biological systems and pose significant health risks (OSHA). Some of the most common toxic metals include arsenic, lead, mercury, cadmium, and thallium. These metals can enter the body through a variety of sources such as contaminated water, food, air, or direct exposure in industrial settings (“Heavy Metal Poisoning”). The impact varies based on the type of metal, level of exposure, and individual factors such as age, overall health, and pregnancy status. Exposure to toxic metals can lead to both short-term and long-term health impacts, making early detection and intervention crucial. This section will focus on the various health effects of toxic metal exposure, starting with immediate symptoms of poisoning and moving into long-term impacts, like neurological damage, organ failure, and cancer risks. It will also address vulnerable populations, like rural communities, children, and industrial workers, who face increased risks due to environmental and occupational exposure. (AC)
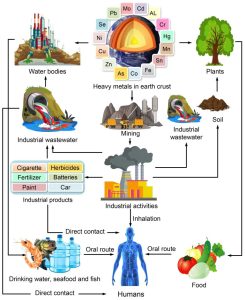
Figure 1 – intoxication mechanisms in humans following exposure to HMS. Adapted from Elnabi et al., 2023
Cadmium-
Cadmium is a heavy metal found naturally in the Earth, like in rocks and marine phosphates. It’s commonly used in industries for making alloys, pigments, and batteries. The use of cadmium has decreased in certain countries over the years, but there is still potential for exposure through sources like cigarette smoke, contaminated food, and working in certain industries (Tchounwou et al.). Cadmium exposure can cause serious health risks, ranging from acute poisoning to chronic disease. Once this metal is absorbed by humans, it will accumulate inside the body throughout life (Jaishankar et al). Acute exposure to cadmium can cause abdominal pain, vertigo, burning sensations, vomiting, muscle cramps, loss of consciousness, and convulsions within 15-30 minutes after ingestion. Chronic exposure is even more damaging because it can lower levels of neurotransmitters in the brain like norepinephrine, serotonin, and acetylcholine. Additionally, cadmium can cause cellular damage by triggering inflammation, generating harmful molecules, and impairing DNA repair, leading to cancer. Studies have also found that exposure may be linked to lung, breast, prostate, bladder, and pancreas cancer (Charkiewicz et al.). (AC)
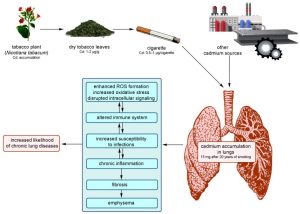
Figure 2- cadmium exposure leading to the development of smoking-related lung disease. adapted from Charkiewicz et al., 2023
Cadmium is especially harmful to the kidneys and bones. Once cadmium enters the body, it tends to accumulate in the kidneys, primarily the renal cortex, where it damages the proximal tubules and leads to early signs of kidney dysfunction, such as proteinuria (the presence of excess proteins in urine) (Charkiewicz et al.). The severity of damage depends on the amount of cadmium present in the kidneys, specifically in the form of cadmium bound to metallothionein (MT), a protein that helps store it. Typically, long-term exposure is detected by measuring cadmium levels in the urine, which indicates how much cadmium has accumulated in the body. In exposed individuals, kidney concentrations can reach as high as 200 mg/kg, with urine levels ranging from about 10-15 micrograms per gram of creatinine, and the acceptable level being 5 micrograms per gram. Overall, It is estimated that about 2.3% of the US population has elevated levels of cadmium in their urine (Charkiewicz et al.). Continued kidney damage can also result in glycosuria (glucose in the urine), aminoaciduria (amino acids in the urine), increased excretion of calcium and phosphorus in urine, increased creatinine concentration, and toxic nephropathy. Because cadmium is excreted from the body very slowly through urine, feces, saliva, or sweat, it tends to remain in the body for years, increasing the risk of long-term damage (Charkiewicz et al.). (AC)
In addition to kidney damage, cadmium also disrupts the body’s ability to maintain healthy bones. Cadmium interferes with the metabolism of essential minerals like calcium, magnesium, iron, zinc, and copper, which leads to bone demineralization, osteomalacia, and osteoporosis. These conditions often cause chronic pain in areas such as the spine, pelvis, and limbs. Many studies have shown a clear link between cadmium exposure and decreased bone mineral density (Charkiewicz et al.). Itai-Itai disease, which means “ouch-ouch” in Japanese, is one of the most well known and severe outcomes of cadmium exposure. It was first identified in Japan’s Jinzu River Basin in the 1930’s, but was not formally recognized until after World War II, when doctors finally began to investigate the pattern of severe bone pain and kidney damage among its local residents. Many people were exposed to cadmium through drinking the Jinzu River water and eating foods such as rice, soybeans, and vegetables grown in polluted areas. Symptoms of the disease include excruciating bone pain, spinal and limb deformities, frequent bone fractures, muscle weakness, and difficulty walking. As the disease progressed, many people became bedridden, and their quality of life significantly decreased. Throughout the 1950’s and 60’s, research confirmed that chronic cadmium poisoning, primarily from industrial waste discharged by the Kamioka Mine, was responsible for the disease. Cadmium contaminated water and rice fields resulted in widespread, long-term exposure among the affected communities. In 1968, after years of investigation, the Japanese government officially recognized cadmium as the cause of itai-itai disease. Itai-Itai disease is an example of the severe and lasting health impacts of chronic cadmium exposure, highlighting the consequences of environmental pollution on both individual health and community well-being (Aoshima). (AC)
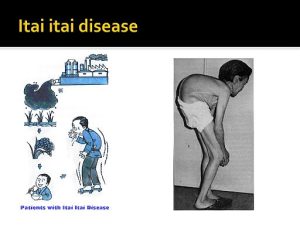 Figure 3- A patient with Itai-Itai Disease. Prepp.in, https://prepp.in/news/e-492-itai-itai-disease-environment-notes. Accessed 5 May 2025.
Figure 3- A patient with Itai-Itai Disease. Prepp.in, https://prepp.in/news/e-492-itai-itai-disease-environment-notes. Accessed 5 May 2025.
Lead-
Lead is naturally occurring in small amounts inside the Earth’s crust. Anthropogenic sources like fossil fuel burning, manufacturing, and mining increase its concentration. It’s commonly found in products like lead-acid batteries, ammunition, metal products, and X-ray shielding devices. Although its industrial use has declined, lead remains a major hazard in older homes with deteriorating lead paint, which can contaminate dust and soil (Tchounwou et al.). Acute lead exposure disrupts normal cellular functioning by competing with calcium, affecting mitochondrial respiration, and impairing neurological tissues (Centers for Disease Control Prevention). It also lowers levels of sulfhydryl groups and glutathione, which leads to the overproduction of reactive oxygen species. Lead further interferes with important enzymes, like those involved in making heme, which can result in anemia (Centers for Disease Control and Prevention). Gastrointestinal symptoms of acute lead exposure include anorexia, constipation, abdominal pain, and vomiting. The central nervous system symptoms can range from muscle weakness to more severe effects like anxiety, delirium, hallucinations, memory loss, seizures, and encephalopathy (Centers for Disease Control and Prevention). (AC)
Going beyond these immediate effects, lead exposure poses significant neuropsychological and long-term health impacts, especially in children and pregnant women. In pregnant women, lead in the blood can increase risk for miscarriage, cause preterm birth, damage the baby’s brain, kidneys, and nervous system, and cause the child to have learning or behavior problems (Centers for Disease Control and Prevention). In children, even low levels of lead exposure can have lasting consequences on brain development. Lead has been linked to many developmental issues such as reduced IQ, shortened attention span, increased antisocial behavior, and lower educational outcomes (World Health Organization). A variety of studies have shown an inverse relationship between blood lead levels and IQ scores- as lead exposure increases, cognitive abilities decrease. One long-term study followed over 1,000 people born in Dunedin, New Zealand, and found that children with high blood levels at age 11 had lower IQ scores by age 38. For every 5 microgram increase in blood lead, participants lost about 1.5 IQ points (Bates). Further, lead exposure has been linked to persistent behavioral issues, including impulsivity, aggression, and reduced emotional regulation. Studies have shown a clear connection between early childhood lead exposure and attention problems, with elevated levels associated with symptoms of ADHD, like hyperactivity, inattention, and difficulty following directions. Research has also shown that children with high lead levels are more likely to display disruptive behavior and involvement with crime later in life. Longitudinal studies have found that early lead exposure correlates with increased rates of arrest, violence, and property offenses in adolescence and adulthood after adjusting for socioeconomic factors (Bellinger et al.). The serious and lasting effects of lead exposure becomes even more real when looking at communities like Flint, Michigan, where thousands were impacted by lead contaminated water. (AC)
In 2014, Flint, Michigan, faced a serious public health crisis when their drinking water was contaminated with lead. This occurred after government officials switched the city’s water supply from Lake Huron to the more polluted Flint River. They then failed to treat the water properly, which caused lead from the pipes to leach into the drinking supply. The people most affected by this environmental disaster were poor and African American populations (Campbell et al.). After the switch, fertility rates dropped by 12% and fetal deaths rose by 58% based on health records from 2008 to 2015. Additionally, babies born at full term during the crisis had lower birth weights, and lead exposure raised the risk of hypertension in pregnant women (National Partnership for Women & Families, 4). The long-term consequences of Flint extend beyond reproductive health, as the children exposed to lead face increased risk of cognitive impairments, behavioral disorders, and other developmental challenges. Dana Brown, who was a junior at the time, remembers struggling to focus. She stated, “I was combining words and numbers a lot…I had to work hard to just learn” (Riley). In 2018, she got a blood test, which revealed elevated levels of lead. Later on, she received a diagnosis for ADHD and dyslexia. The effects of lead exposure in Flint, Michigan, continue to impact the health and development of its residents, highlighting the consequences of environmental injustice. (AC)
Arsenic-
Arsenic is a widespread element found in low concentrations in nearly all environmental sources such as soil, water, and air. Humans can be exposed to arsenic through ingestion, respiration, and dermal absorption (Huang et al.). Acute arsenic poisoning can cause severe gastrointestinal symptoms, including nausea, vomiting, abdominal pain, and diarrhea. At high doses, toxicity can lead to dehydration, organ failure, and even death within hours or days. Other reported effects include skin rashes, psychosis, seizures, and peripheral neuropathy. Severe cases may also lead to renal failure, cardiomyopathy, and encephalopathy (Ratnaike). (AC)
Further, arsenic is classified as a Group 1 human carcinogen by the International Agency for Research on Cancer (IARC). Its compounds have been shown to inhibit DNA repair, induce chromosomal abnormalities, and cause cell transformation in both human and rodent studies. Long-term exposure to arsenic has been linked to cancer development, with evidence suggesting that arsenic disrupts DNA methylation, alters gene expression, and activates certain signaling pathways, which contributes to the carcinogenic process (Tchounwou et al.). (AC)
Studies show a strong association between arsenic contaminated drinking water and increased risks of developing skin, lung, bladder, liver, and kidney cancers (Speer et al.). Inhaled inorganic arsenic increases the risk of lung cancer, especially among workers in mining, smelting, chemical industries, and nearby residents. Studies have shown that exposure activates AKT and mTOR, proteins involved in cell growth and survival. AKT helps regulate cell growth and survival, while mTOR controls cell growth and protein synthesis. These proteins work together to help cells grow and divide uncontrollably, which is a key feature of cancer development. Chronic arsenic exposure also affects the skin, leading to skin issues like keratosis, hyperpigmentation, and skin cancer, as well as arsenicosis, a condition that causes thickening and hardening of the skin. Additionally, arsenic serves as a risk factor for bladder cancer, one of the most common cancers worldwide. Epidemiological studies have shown a clear connection between high levels of arsenic in drinking water and bladder cancer, which led to the World Health Organization reducing the recommended levels of arsenic concentration in drinking water from 25 micrograms per liter to 10 micrograms per liter (Palma-Lara et al.). (AC)
In Bangladesh, the contamination of the groundwater is known as the largest mass poisoning in history, caused by arsenic leaching into tube well water used for drinking and cooking. Before the 1970’s, residents used surface water for drinking and related activities, but this resulted in several types of diarrheal diseases because the water was contaminated with pathogens. To reduce this problem, the government installed tube wells, but many years later, it was discovered that the water from the tube wells contained arsenic in toxic levels. At this point, it was too late, and millions of people had already been exposed. An estimated 35 million people in Bangladesh have consumed arsenic contaminated drinking water for decades (Choudhury et al.). The health consequences of long-term exposure resulted in increased incidence of cancer, cardiovascular disease, and respiratory illness. Specifically, a 12 year long study found a link between arsenic exposure and skin cancers in Bangladesh, with Basal Cell Carcinoma and Squamous Cell Carcinoma being the most common forms. The results indicated a higher rate of these cancers among men because they were more likely to participate in outdoor labor and consume more water per day than others. In some areas of Bangladesh, such as Chandpur, Gopalganj, Madaripur, and Shariatpur, arsenic concentration in drinking water has exceeded 50 micrograms per liter, with levels even reaching as high as 500 micrograms per liter (Choudhury, et al.). It’s estimated that about 5.6% of deaths in Bangladesh are attributed to arsenic exposure, and arsenic related disease contributes to about 0.3% of the total burden of disease (Ahmad et al.). Arsenic exposure in Bangladesh is another example of how environmental health hazards can accumulate over time, causing a severe public health crisis. (AC)
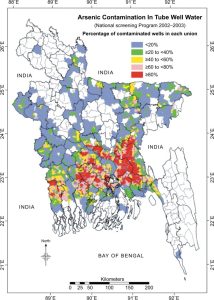
Figure 3- Arsenic contamination map of Bangladesh. adapted from Ahmad et al., 2018
Mercury-
Mercury is a heavy metal that occurs in three forms: elemental, organic, and inorganic. These forms of mercury are present in water sources like lakes, rivers, and oceans, where they cause disturbance to aquatic life. Consuming these contaminated animals, such as fish, is the major route of human exposure to methylmercury (Jaishankar et al.). Additionally, it’s used in electrical manufacturing, dentistry, and various industrial processes. Mercury is a widespread environmental pollutant that affects both humans and animals (Tchounwou et al.). Acute exposure to metallic mercury typically occurs when it’s spilled or products that contain it break, causing it to be exposed to the air. Inhalation of its vapor can lead to symptoms such as tremors, mood swings, irritability, insomnia, muscle weakness, headaches, sensory disturbances, and mental function impairments. Increased levels of exposure may cause kidney damage, respiratory failure, and potential death (US Environmental Protection Agency). The link between mercury exposure and cancer is controversial. Some studies suggest it damages DNA through oxidative stress, potentially leading to mutations and carcinogenesis, but others find no clear link (Tchounwou et al.). (AC)
An example of mercury’s impact on human health can be demonstrated through Minamata Disease, a methylmercury food poisoning that occurred in Japan during the 1950’s and 1960’s. During this time, a chemical company located in Minamata, Japan dumped industrial wastewater containing methylmercury into the Minamata Bay. It then accumulated in organisms such as fish and shellfish, which was a popular food for the locals. As the residents consumed the contaminated seafood, they ingested increasing amounts of methylmercury, which led to a variety of neurological symptoms. Some of these symptoms included ataxia (loss of coordination), numbness in the limbs, muscle weakness, vision and hearing impairment, and speech difficulties. Additionally, children born to mothers exposed to methylmercury throughout their pregnancy often experienced congenital Minamata Disease, characterized by physical deformities, seizures, and other developmental delays. In 1968, Japan officially recognized methylmercury as the cause, but by then, thousands had already been impacted- many people died, and others were left with lasting disability. Years later, in recognition of the devastating health and environmental effects caused by mercury, The United Nations Environment Programme (UNEP) created the Minamata Convention on Mercury in 2013. This global treaty aims to reduce mercury pollution worldwide by decreasing emissions from industrial sources, managing contaminated sites, and phasing out the use of mercury in products (Environmental Literacy Council). Minamata Disease can serve as a reminder of just how harmful toxic metals can be to human health, and why continued global efforts to reduce exposure are so important. (AC)
Thallium-
Thallium comes from both natural and anthropogenic sources, leading to increased levels in the environment. It’s released into the air through industrial processes like coal burning, cement production, and metal burning. Once in the air, thallium can travel long distances before entering soil or water. Certain forms of thallium can dissolve in water and seep into the groundwater, causing a contamination risk. Plants can absorb thallium from contaminated soil, allowing it to enter the food chain and build up in animals and humans, potentially leading to serious health effects (Karbowska). (AC)
Acute thallium poisoning causes gastrointestinal symptoms such as severe abdominal pain, vomiting, nausea, and diarrhea within hours or up to two days after ingestion. Thallium primarily affects the nervous system, which leads to rapid peripheral neuropathy that starts in the feet/legs and moves to the hands. Severe cases have resulted in disorientation, coma, seizures, pulmonary edema, heart failure, and psychiatric disorders, like psychosis and depression (Fujihara and Nishimoto). Long-term effects following acute exposure can lead to altered blood chemistry, hair loss, and damage to the liver, kidneys, intestine, and tissue in the testes. The most well-known symptom of thallium poisoning is alopecia, causing hair loss of more than 100 hairs per day, 2-3 weeks after exposure. Additionally, dry and scaly skin can be experienced 2-4 weeks after exposure. Chronic thallium exposure also leads to alterations in the brain, spinal cord, and peripheral nerves (Fujihara and Nishimoto). The wide range of harmful effects caused by thallium poisoning highlights how dangerous this substance is, making it crucial to prevent exposure and catch it early to avoid long-term effects. (AC)
In pregnant women, thallium can pass through the placenta to the developing fetus. This exposure increases the risk of complications like miscarriage, low birth weight, and preterm birth. While some babies may be born with no immediate symptoms, others may experience hair loss or developmental delays later on. Studies have also linked high thallium exposure to an increased risk of ADHD and lower IQ in children (Fujihara and Nishimoto). These risks emphasize the need to avoid thallium exposure during pregnancy to protect the mother and child. (AC)
Overall, cadmium, lead, arsenic, mercury, and thallium can cause significant health impacts on humans. They can enter the body through contaminated air, water, food, and consumer products, accumulating over time. Exposure is associated with a wide range of acute and chronic health effects, including neurological damage, kidney dysfunction, cardiovascular disease, developmental delays, and even cancer. Because many of these metals accumulate in the body, even low level exposure can lead to serious long term health risks, making public health protection and regulations essential. (AC)
Vulnerable popualtions-
Identifying high-risk populations is essential for preventing metal toxicity and reducing long-term health effects. These groups often face a combination of environmental, social, and occupational conditions that increase their risk of exposure. Some populations at highest risk include industrial workers, children in poor housing, heavy fish eaters, and those living near highways, farms, or industrial sites (Landrigan et al.). (AC)
Children are especially vulnerable to metal toxicity due to their higher exposure levels and developing metabolic systems. They consume more food, water, and air per kilogram of body weight compared to adults, which increases their exposure to metals in the environment (Landrigan et al.). Additionally, their developing metabolic systems make it harder for them to detoxify and process these toxic substances. This can lead to health effects such as chronic disease and developmental issues. The risk is especially high for children in low and middle-income countries because they are becoming rapidly industrialized with few regulations in place (Landrigan et al.). (AC)
Even in the United States, disparities still persist. Although lead poisoning has declined, poor and minority children are disproportionately affected. They are more likely to live in older houses with lead chips, contaminated dust, and lead pipes. These conditions increase their risk of lead exposure, especially during early childhood when their bodies are still developing and are more vulnerable to toxins. National surveys have shown that low-income children, non-Hispanic Black children, and children living in houses built before 1946 have significantly higher blood lead levels (Gochfeld and Burger). For example, in Rochester, New York, nearly half of Black children were found to exceed the blood level threshold of concern, compared with just 6% of white children (Gochfield and Burger). Additional risk factors include living in small housing units, frequent hand-to-mouth behavior, and nutritional deficiencies. Despite overall progress of decreased blood-lead levels, these disparities emphasize the need for improved public health efforts to protect vulnerable children from lead exposure and the long-term impacts that come with it. (AC)
Low-income, minority, and rural communities who rely on non commercial, wild-caught food sources also face elevated exposure to mercury and other metals. Cultural food practices, like high fish consumption in Asian American communities or crab and deer in black and white populations can increase risk of exposure (Gochfeld and Burger). Overall, lower income was linked to higher consumption of these potentially contaminated foods. These findings highlight the importance of considering cultural and socioeconomic factors when assessing risk and developing public health interventions. (AC)
Rural communities face additional layers of risk to toxic metal exposure. They are often located near farms, feedlots, mines, and waste sites, which increases risk of exposure to pesticides, water pollutants, and metals like arsenic. Homegrown produce and livestock can also be exposure pathways due to being grown in contaminated soil and water (Gochfield and Burger). Rural communities face unique and often overlooked exposure routes that can contribute to their vulnerability to toxic metals. (AC)
Industrial workers are especially vulnerable to toxic metal exposure due to their work environments. Industrial processes, like welding, alloy smelting, and construction lead to inhalation and exposure of metal dust, fumes, or vapors. Occupational exposures to metals like lead, mercury, cadmium, and arsenic are common in these settings, and can put workers at risk of poor health effects. A study done by Boston University showed that construction workers had higher levels of arsenic, chromium, manganese, nickel, and tin dust in their homes compared to workers in janitorial or auto repair occupations (Mckoy). This suggests that take home contamination is a serious risk of exposure because the particles left on the skin, clothing, and personal items cannot only endanger workers, but their families as well. (AC)
Protecting these vulnerable populations requires a targeted approach that addresses both direct exposures and the social factors that contribute to increased risk. Public health interventions should be created with the needs of vulnerable groups, such as the ones above, in mind. (AC)
Prevention efforts-
Current US regulations for toxic metals are designed to protect public health by limiting exposure to substances like lead, mercury, cadmium, and arsenic. Agencies like the Environmental Protection Agency set strict limits on the amount of these metals in the environment through various regulations, such as the Safe Drinking Water Act, which sets maximum contaminant levels in public water systems. Additional advancements have been the removal of lead based paint in 1978 and the removal of lead in gasoline in 1996. The US Superfund programs were also implemented to identify and clean up extremely contaminated waste sites across the country, many of them being contaminated with toxic metals (US Environmental Protection Agency). However, even with these and many other regulations in place, contamination through food, water, soil and air still persists, especially in historically industrial areas. For example, in the Tri-State Mining District, which includes southeast Kansas, southwest Missouri, and northeast Oklahoma, Lead and Zinc were actively mined from 1850’s up until the industry closed in 1970. Many decades later, toxic metal contamination remains in the soil, groundwater, and sediments, and these areas are now considered “Superfund” sites by the EPA. In these sites, there is an abundance of waste materials (Pb, Cd, and Zn), mining shafts, and tunnels left, which contaminates groundwater and soil. A study found that children living near chat piles are still at risk for toxic metal exposure. It was discovered that the dust in the homes had higher concentrations of Zn, Pb, Cd, and As, compared to dust in the nearby soil. Metal particles from chat sources can contaminate homes through the wind carrying particles. So, families are still being affected, even those who do not live directly near a mining site. Additional studies have shown that there are many sources for residents to be exposed to metal contaminants. In Jasper County, Missouri, 14% of children had elevated lead blood levels compared to the control group, indicating a serious public health concern. Despite the closure of mining operations over 50 years ago, the Tri-State Mining District continues to suffer the effects of toxic metal pollution. The presence of heavy metals in the dust, soil, water, and air highlights the need for more effective regulations, cleanup efforts, and public health monitoring to mitigate exposure and protect vulnerable populations (Park et al.). (AC)
Globally, prevention efforts vary in effectiveness. In Bangladesh, the government has worked to label unsafe wells, promote safe water sources, and raise public awareness surrounding arsenic, but millions of people still rely on arsenic contaminated water, especially in rural areas. (AC)
Toxic metal exposure remains a significant public health issue in the United States and around the world. Vulnerable populations, like children, low income communities, rural communities, and industrial workers face increased risks due to occupational exposure, environmental hazards, and socioeconomic disadvantages. Although US regulations like the Safe Drinking Water Act and Superfund programs have made progress in reducing exposure, continued contamination in places like the Tri-State Mining District shows that more effective monitoring, cleanup, and community based interventions are still needed. Countries like Bangladesh continue to struggle with arsenic exposure, even after years of prevention efforts. In contrast, Japan’s response to mercury poisoning helped create international efforts, eventually leading to the Minamata Convention, which shows how global response can cause meaningful policy change.(AC)
