3 Monitoring Devices
Pulse Oximetry:
- The pulse oximeter is a measures the systemic oxygen saturation. In other words, it detects which percentage of hemoglobin molecules are carrying oxygen in the arterial/systemic bloodstream.
- In order to give an accurate reading, the device needs to be able to detect pulsatile blood flow. Therefore, the device needs adequate tissue perfusion to be reliable.
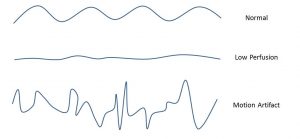
- For that reason, it is important to ensure a good waveform before interpreting the saturation. A good waveform should show a steady undulation in sync with the ECG tracing (See “Normal” below)
- If the monitor is reading unexpectedly low or is unable to pick up the oxygen saturation at, you should rule out decreased tissue perfusion. Inaccurate readings can also be from motion artifact, which is especially prevalent in infants and toddlers.
- The reading is unreliable in carbon monoxide and methemoglobin poisoning (low PaO2 with normal sat), so it is always important to consider this in patients at risk of those illnesses.
Arterial blood pressure monitoring:
- An arterial line is an invasive way to monitor blood pressure both continuously and more accurately. Common sites for arterial lines include the radial arteries, femoral arteries, and less often in the dorsalis pedis and posterior tibial arteries.
- The blood pressure reading can be erroneous in a number of settings, including vasospasm, patient movement, or if the transducer is not lined up with the patient’s phlebostatic axis. You should ensure the waveform of the arterial line is appropriate before interpreting pressures. The wave form (see figure below) should have an appropriate upswing to the systolic notch. The bump on the downswing is the dicrotic notch and represents closure of the aortic valve.
- Pay attention to both pulse pressure and the consistency of the systolic notch. A wide pulse pressure could indicate chronic anemia, PDA, or vasodilatation. A narrow pulse pressure can be seen in status asthmaticus, cardiac tamponade, or dehydration. In addition, a variable peak in the systolic notch between inhalation and exhalation, typicall more than 10% and known as pulse pressure variability, can indicate intravascular volume depletion.
- If the arterial waveform is blunted, reading inaccurate blood pressure, and you believe it is due to arterial spasm, you can add papaverine 30-60 mg to the arterial line fluids.

Central venous pressure monitoring:
- The central venous pressure (CVP) reflects the amount of blood returning to the heart, known as the “preload,” as well as the function of the right ventricle. For example, CVP can be elevated when the volume of blood returning to the right heart is high or when the right heart is functioning poorly (causing “backup” of venous return and increasing the pressure reading).
- The reading is obtained by attaching a pressure transducer to a central venous catheter.
- Just as with arterial lines, it is important to evaluate the CVP waveform. A normal CVP tracing has 3 positive waves (a,c,and v) and 2 negative waves (x and y). The “a” wave is caused by atrial contraction, the “c” wave by ventricular contraction against a closed tricuspid valve, and the “v” wave is caused by atrial filling. The “x” descent is due to the tricuspid valve being pulled away from the right atrium by the contracting ventricle, while the “y” descent occurs as the tricuspid valve opens and blood enters the ventricle.
- Also similar to arterial lines, the CVP transducer should be appropriately leveled and zero’d, and the reading should be obtained at end expiration.
- A high CVP could indicate tricuspid regurgitation, tricuspid stenosis, heart failure, or elevated intrathoracic pressure (essentially anything that cause blood flow or pressure to be pushed back towards the great veins instead of forward toward the lungs.
- A Low CVP could indicate hypovolemia or distributive shock (anaphylaxis)
- A normal CVP is, generally, 2-6 mmHg although this can vary from patient to patient depending on right heart function.
- We generally use heparinized normal saline fluids @ 2-3cc/hr to prevent clotting in the line.

Cerebral & Renal Somenetics
- Somenetics, or Near-Infrared Spectroscopy (NIRS), uses the near-infrared region of the electromagnetic spectrum to measure regional tissue perfusion and oxygen delivery.
- The sensors are typically placed on the forehead (brain) and flank (kidney) but can theoretically be placed anywhere. The monitor will give you a regional oxygen saturation for those organs.
- The absolute number isn’t as helpful as the trend over time. BY following that trend you can assess the adequacy of cardiac output and oxygen delivery as the patient’s illness evolves.
- This monitoring device is particularly useful in post-op cardiac patients and in children with shock, two populations in which ensuring adequate cardiac output and oxygen delivery is paramount to recovery.

End-Tidal CO2 monitor:
- An end-tidal carbon dioxide monitor measures the CO2 level of exhaled air when the patient is mechanically ventilated. The device is attached to the ventilator tubing where it connects to the endotracheal tube, and gives a continuous reading based on each breath.
- Initially, you need to ensure that the reading correlates with the actual pCO2 from a blood gas. Once that it is done, and assuming they correlate, you can then make ventilator adjustments or follow the patients progress ( in terms of ventilation and CO2 clearance) by following the end-tidal reading instead of getting frequent blood gases.
- A big discrepancy between end-tidal CO2 and the blood gas may be due to increase in dead space ventilation due VQ mismatch. The absence of an end-tidal reading could be due ET tube obstruction or unplanned extubation.
- Keep in mind that the reading is unreliable in presence of air leak around the ET tube.

ICP Monitoring:
- Monitoring of intracranial pressure (ICP) can be done via multiple devices: Subdural bolts and ventriculostomy catheters (aka EVD) are most common in our PICU.
- ICP monitoring is indicated in patients at risk for elevated intracranial pressure, which can result in brain ischemia or, in severe cases, brain herniation.
- Both devices are placed by a neurosurgeon. The subdural monitor gives a continuous reading of the ICP. An EVD is a catheter placed in to a lateral ventricle, which can then drain CSF from the lateral ventricle if the pressure in the ventricle increases above a set-point. Using an EVD, on the other hand, the actual ICP is measured intermittently. This is done by using a three-way stopcock to close off the catheter towards the drainage system but to open the catheter towards a pressure transducer which then reads the pressure. Because the stopcock needs to be manually closed to the catheter and opened towards the transducer by the nurse, and because typically the catheter is left open in order to allow CSF to drain, an EVD only gives an intermittent “closed” ICP reading.
- Normal ICP is considered to be 0-10 mmHg. An ICP > 20 is abnormal and dangerous, and needs to be treated.
- ***Pressure spikes that go up and stay up are of most concern and need treatment!
- Another important number to pay attention to is the Cerebral Perfusion Pressure (CPP). This represents the amount of driving pressure (mean arterial pressure or MAP) used to push blood up to the brain. In order for blood to flow to the brain, this pressure must overcome any resistance pressure in the skull (ICP). Thus, the CPP is the difference betweent he driving pressure and resistance, and is calculated by taking the mean arterial pressure (MAP) minus the ICP Goal. For example, if a patients MAP is 90 and the ICP is 15, then the CPP is 75 (90 minus 15). Our general CPP goals are > 50 for infants, > 60 for most children, > 70 for adults.

Telemetry:
- Continuous ECG monitoring allows for assessment of heart rate and rhythm, ischemia, and conduction defects.