5 Neurology
Glascow Coma Scale (GCS) for Pediatrics:
The GCS score is used to assess mental status following traumatic injury.
In an intubated patient, one point is given for verbal response but the final score is reported with a “T.” For example, if an intubated patient opens her eyes to speech (3) and withdraws to painful stimuli (4), her GCS score would an “8T.”
A CGS score of 8 or less suggests severe traumatic brain injury and the patient likely requires intensive therapy including airway control/maintenance. A popular phrase to help you remember is “GCS less than 8, then intubate.”
| Child | Infant | Score | |
| Eye Opening | Spontaneous | Spontaneous | 4 |
| To speech | To speech | 3 | |
| To pain | To pain | 2 | |
| None | None | 1 | |
| Best Verbal Response | Oriented, Appropriate | Coos and babbles | 5 |
| Confused | Irritable, cries | 4 | |
| Inappropriate words | Cries in response to pain | 3 | |
| Incomprehensible sounds | Moans in response to pain | 2 | |
| None | None | 1 | |
| Best Motor Response | Obeys commands | Moves spontaneously and purposefully | 6 |
| Localizes painful stimuli | Withdraws in response to touch | 5 | |
| Withdraws in response to pain | Withdraws in response to pain | 4 | |
| Flexion in response to pain | Abnormal flexion posture to pain | 3 | |
| Extension in response to pain | Abnormal extension posture to pain | 2 | |
| None | None | 1 | |
| Total Score | 3–15 |
Traumatic Brain Injury:
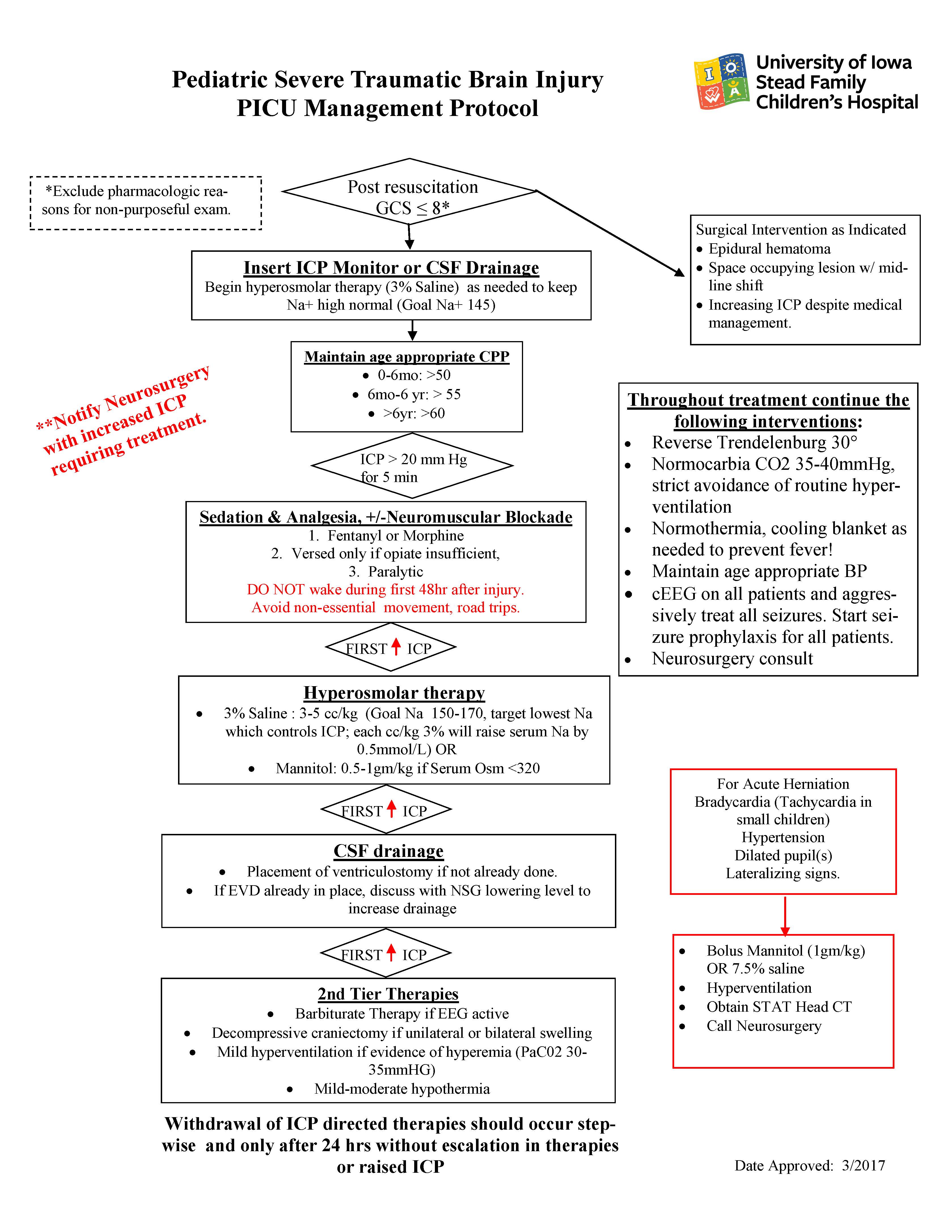
The goal in traumatic brain injury is to limit the potential for secondary brain injury by ensuring adequate oxygen delivery, done by ensuring both adequate oxygen availability and by limiting the brain’s need for oxygen (metabolic demand). An important way to monitor this goal is by limiting the cerebral edema to the greatest extent possible and by monitoring the intracranial pressure. Ways to diminish metabolic demand and cerebral edema include:
- Prevention of fever (Scheduled acetaminophen)
- Prevention of seizures (Prophylactic Keppra with continuous EEG monitoring)
- Maximize venous drainage of intracranial blood (Head of bed at 30 degrees, head in midline)
- Good sedation, pain control, and, potentially, pharmacologic paralysis
- Tight control of mechanical ventilation (pCO2 goal 35-40, Saturation >92%)
- Maintain ICP < 20
- Age appropriate blood pressure, but CPP > 50/60/70 for infants/children/adults
- Hyperosmolar therapy, with goal serum sodium 145 or greater (may need to be higher based on ICP readings)
Emergenct therapies for impending brain herniation include:
- Bolus of 3% saline
- Bolus of sedative, pain, or paralytic medication
- Consider burst suppression with pentobarbital infusion
- Mannitol therapy
- Brief hyperventilation
- Hemicraniectomy by neurosurgery
Status Epilepticus:
Initial Management of Status Epilepticus (Neurology Pocket Card, Feb 2019):
Impending SE, 5 minutes
- Lorazepam (Ativan) 0.1 mg/kg IV (max 5 mg) over 1 min
- Nasal midazolam 0.2mg/kg/dose
- Rectal diastat 0.5mg/kg (dose by age and weight)
Allow 5min to determine whether seizure terminates. During that time, stabilize the airway, breathing, and hemodynamics as needed. Continuously monitor vital signs. Check bedside glucose.
Consider obtaining labs: BMP, Ca, Mg, Phos, glucose, CBC, LFTs, toxicology screen, and AED level if applicable
Established SE, 5-10 minutes
- Repeat benzodiazepine dosing
- Consult/call Pediatric Neurology
For children:
- Fosphenytoin 20 mg PE/Kg IV/IM at 3 mg PE/Kg/min via peripheral IV line (maximum 1500mg PE) (consider avoiding with known gen epilepsy)
- check phenytoin level 2 hours after infusion
For infants:
- Phenobarbital 20mg/kg IV
Initial refractory SE, >10 minutes:
- Consider 10mg/kg fosphenytoin or phenobarbital
- Or administer second drug
- levetiracetam 60mg/kg IV or
- valproate 40 mg/kg at 5 mg/kg/min (avoid valproate in children <2 years of age)
Loading Doses:
| Drug | Dose (IV) | Comment |
| Levetiracetam (Keppra) |
|
Max dose: 2500 mg |
| Phenobarbital |
|
May cause hypotension Max dose: 1Gm |
| Phenytoin or Fosphenytoin |
|
Max dose: 1Gm, |
*PE Phenytoin Equivalents
Continuous Infusions:
| Midazolam | 10-200 mcg/kg/min | Titrate to effect (seizure cessation) |
| Pentobarbital | 1–5 mg/Kg/hr | Goal: Seizure cessation or “Burst Suppression” |
| Propofol | 25–100 mcg/Kg/min | Short term use only due to potential for propofol infusion syndrome |