Blood Glucose Monitoring
Routine blood glucose monitoring with a bedside point-of-care (POC) glucometer is needed for all patients admitted to the hospital with insulin-dependent diabetes mellitus (e.g. T1DM, T2DM, CF-related DM, etc.).
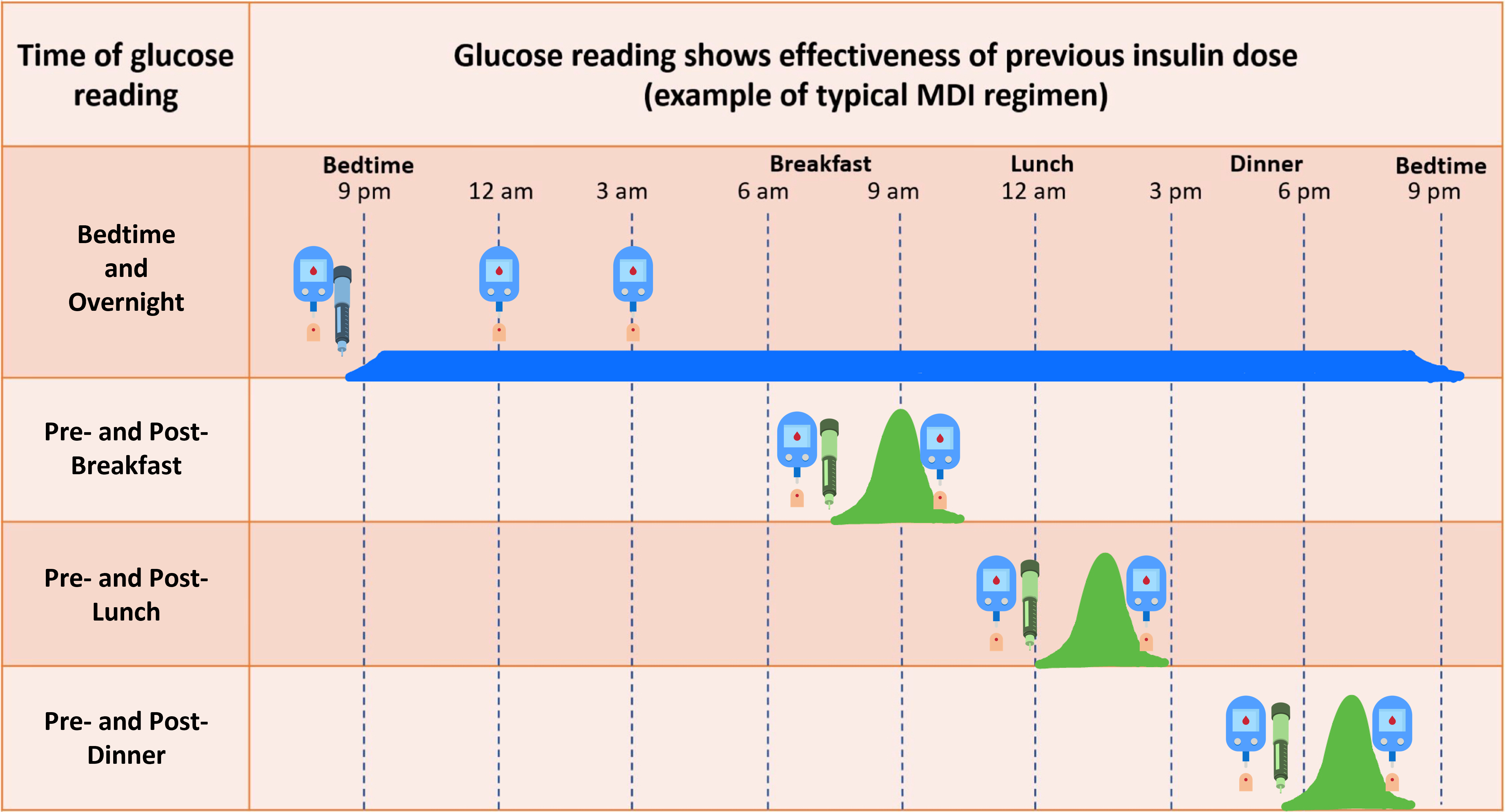
Routine blood glucose monitoring is performed 9 times per day at the following “protocolized” times:
- Within 15-30 minutes before meals (3 x per day)
-
- These are preprandial blood sugars
- Two hours after each meal (3 x per day)
- These are postprandial blood sugars
- “Bedtime” (~2100)
- Midnight (0000)
- 3 AM (0300)
Inpatient blood glucose monitoring for patients with non-insulin-dependent Type 2 diabetes usually includes:
- Fasting AM blood glucose prior to breakfast
- A 2-hour postprandial blood glucose after lunch or dinner
A Note on CGMs:
- CGMs are not currently FDA approved for inpatient use as the accuracy of these devices may be drastically impacted by acute illness (patients are in a state of disequilibrium) and various medications.
- If a patient is allowed to continue wearing their CGM:
- POC blood glucose must also be obtained and logged by nursing during their admission as CGM readings may not be reliable.
- Additional POC blood glucose checks are needed to confirm alarms/alerts by the device.
- If a patient is allowed to continue wearing their CGM:
- CGMs must be removed prior to MRIs and prior to x-ray radiation (CT or X-rays)
The frequency of bedside blood glucose monitoring by POC blood glucose checks changes under the following conditions:

Additional blood glucose checks may be needed outside of the routine checks that were discussed above.
Keep the following rules of thumb in mind and you will never go wrong:
Blood Glucose Checks at “Non-protocolized” times:
- When in doubt, check a blood sugar
- It is always safer to check blood sugar more often (or sooner than the next scheduled check) if you have clinical doubts or concerns about a patient
- Before ANY rapid-acting insulin administration
- This includes any non-protocolized insulin administration
- It is always safer to determine where the blood sugar is starting from as it may help guide how much insulin is to be given and the timing of the follow-up blood glucose check
- 2-3 Hours AFTER any rapid-acting insulin administration
- This includes insulin delivered at non-protocolized times or insulin given for ketone corrections
- Why?
- Rapid-acting insulin’s peak action time is 1-2 hours and the duration of action is 3-4 hours after administration. Checking a blood sugar 2-3 hours after insulin administration allows you to see how the patient’s blood sugar “responds” to the dose that was given and monitors for the development of hypoglycemia.
- For any symptoms of hypoglycemia or severe hyperglycemia or ketosis
- Hypoglycemia should be treated immediately if present
- Hyperglycemia, if causing significant symptoms should be addressed and the patient should check for the presence of ketones
Quiz Yourself:


Feedback/Errata