Laboratory Evaluation
Diagnosing diabetes mellitus and determining if there is associated DKA requires laboratory evaluation.
Since a patient with suspected new-onset diabetes with clinical symptoms is considered a pediatric medical emergency, prompt laboratory testing is required, even in children who have features more consistent with Type 2 diabetes.
“Prompt,” in this case, means labs are performed as soon as possible, on the same day of presentation, with follow-up of these labs on the same day of presentation to ensure the appropriate escalation of care based on the lab results.
Minimum laboratory evaluation for patients with suspected diabetes includes labs that confirm the presence of hyperglycemia and/or the presence of ketones. These labs include:
- Plasma glucose (fasting or random), ideally not by point of care (POC – fingerstick) methods
- Urinalysis or urine dipstick assessing for glucosuria and ketonuria
The presence of ketones in the setting of hyperglycemia, regardless of reported symptoms, should prompt further evaluation for diabetic ketoacidosis by obtaining the following:
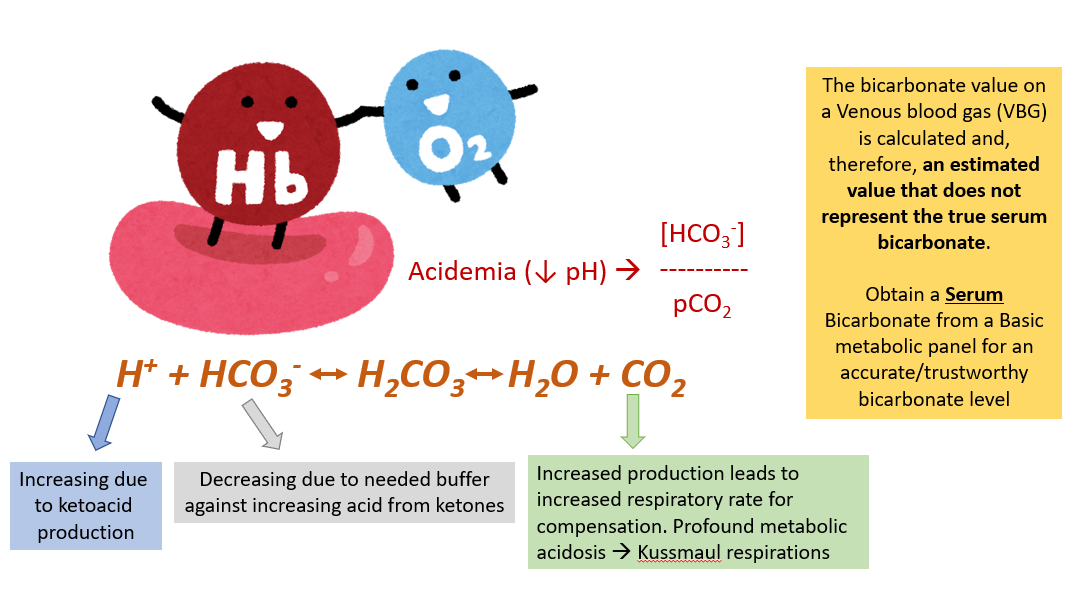
- Basic metabolic panel (includes plasma glucose and serum bicarbonate)
- Venous blood gas
Ketosis in Diabetes Mellitus Leads to Shift in Acid-Base Balance
For patients presenting to the emergency department with hemodynamic instability, altered mental state, or coma, additional laboratory testing should be obtained to evaluate for other underlying causes of these presenting symptoms, many of which are triggers for DKA.
It is easy to forget that seizures, infections, pancreatitis, intoxication, and ingestions can present in the same way!
Therefore, consider the following additional labs:
- CBC with differential
- +/- blood cultures (especially if presenting with hypotension or other signs of shock)
- Ionized (or total) calcium, phosphorus, and magnesium (to evaluate for other common electrolyte derangements that are common in the setting of DKA)
- Amylase and Lipase (if presenting with nausea/vomiting and abdominal pain symptoms consistent with pancreatitis)
- Drugs of abuse panel (if suspecting intoxication)
- Tylenol/Salicylate levels (if suspecting ingestions)
Lastly, for new-onset diabetes patients, additional laboratory testing is often helpful in further differentiating Type 1 and Type 2 diabetes. These should be obtained upon inpatient admission if they were not previously obtained.
These labs include:
- C-peptide
- +/-Total insulin (only if the patient hasn’t been started on exogenous insulin)
- Hemoglobin A1c (HbA1c)
- Islet and β-cell pancreatic autoantibodies:
- o Glutamic acid decarboxylase antibody (GAD Ab)
- o IA-2 antibody
- o Insulin antibodies
- o Islet cell antibody, IGG
- o +/- Zinc transporter 8 antibody (Zn8Ab)
- TSH with reflex-free T4 (as autoimmune hypothyroidism can be comorbid with T1DM)
- TTG-IgA (as celiac disease can be comorbid with T1DM)
Quiz Yourself:
Bibliography:
- Libman I, Haynes A, Lyons S, Pradeep P, Rwagasor E, Tung JY, Jefferies CA, Oram RA, Dabelea D, Craig ME. ISPAD Clinical Practice Consensus Guidelines 2022: Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr Diabetes. 2022 Dec;23(8):1160-1174. doi: 10.1111/pedi.13454. PMID: 36537527.
- Glaser N, Fritsch M, Priyambada L, Rewers A, Cherubini V, Estrada S, Wolfsdorf JI, Codner E. ISPAD clinical practice consensus guidelines 2022: Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2022 Nov;23(7):835-856. doi: 10.1111/pedi.13406. PMID: 36250645.
Images/Figures:
- Figure 1 Image Attribution: “Blood Drop Cliparts #2784471″ by https://clipart-library.com and “Clinical Urine Tests Computer Icons Drug Test Urine Collection Device” by kesha0129 at https://imgbin.com/
- Figure 2 : Text in the figure added by Dr. Alex Tuttle and includes the following image: Image attribution: “Hemoglobin Oxygen Venous Thrombosis Iron Blood” by hyperyer7415 at https://imgbin.com/


Feedback/Errata