Calculating Basal and Bolus Insulin Needs
- For children >3 years of age, basal insulin needs are 50% of the TDD.
- Children <3 years of age are generally very insulin sensitive and often require more bolus than basal insulin. Therefore, discuss using 20-40% of the TDD for the initial basal insulin dose.
Example: Calculating Basal Insulin Dose
- For the 6-year-old from our previous example with a TDD of 10.2 units/day
- Basal insulin = 0.5 x TDD
- Basal insulin = 0.5 x 10.2 units/day
- Basal insulin = 5.1 units/day
- Round to the nearest 0.5 units (if using vial/syringe) OR the nearest whole unit (if using insulin pens)
- Thus, this patient needs 5 units of long-acting insulin
- Round to the nearest 0.5 units (if using vial/syringe) OR the nearest whole unit (if using insulin pens)
- For the 14-year-old from our previous example with a TDD of 44.3 units/day
- Basal insulin = 0.5 x TDD
- Basal insulin = 0.5 x 44.3 units/day
- Basal insulin = 22.2 units/day
- After rounding (per the above example), this patient needs 22 units of long-acting insulin
For children > 3 years old, 50% of the patient’s total daily insulin needs come from basal insulin; the other 50% comes from bolus insulin. This bolus insulin is usually divided across three meals per day (breakfast, lunch, and dinner) and thus represents the initial insulin needed for carbohydrate coverage.
Keep in mind that families are educated on one of two methods for carbohydrate coverage:
- Constant Carb Diet
- Insulin to Carbohydrate Ratios
Each method has its advantages and disadvantages and is discussed in further detail below.
Constant Carb Diet:
This method involves giving a fixed dose of insulin for a fixed amount of carbohydrates per meal.
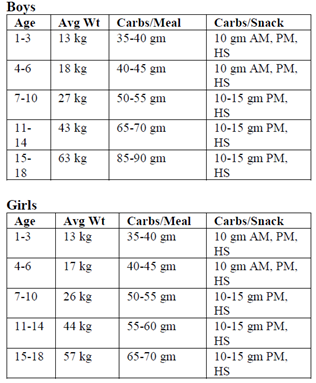
Each patient with new-onset diabetes will meet with a dietician; however, the chart in Figure 4 is a good place to start when estimating the number of carbohydrates per meal based on a patient’s sex, age, and weight.
The amount of insulin per meal is determined by splitting 50% of the TDD among (typically) three meals per day. Children who are bolus or G-tube dependent may need additional boluses or use of different types of insulin.
Example A: Calculating Units of Insulin Needed per Meal for a Constant Carb Meal Plan
- Using the 17kg, 6-year-old, male patient from our prior example with a TDD of 10.2 units/day:
- 50% of the TDD/ 3 meals per day = units of insulin per meal
- (10.2 u/day x 0.5)/ 3 = 1.7 units per meal
- Round to the nearest half-unit, as this is the most accurate dose that can be delivered by an insulin syringe or an insulin pen. Thus, = 1.5 units per meal
- Using the chart in Figure 2 we find that our patient would need 1.5 units of insulin per meal consisting of a target of 40-45g of carbohydrate (CHO) per meal.
- Using the 59kg, 14-year-old, female patient from our prior example with a TDD of 44.3 units/day:
- 50% of the TDD/3 meals per day = units of insulin per meal
- (44.3 u/day x 0.5)/3 = 7.4 units per meal
- Rounds to 7.5 units per meal (per rounding rules above)
- Using the chart in Figure 2, our patient would need 7.5 units of insulin per meal consisting of a target of 60-65g CHO per meal
The constant carb diet method is advantageous for families that may have difficulty with the calculations needed for the insulin to carbohydrate method.
The disadvantage of this method of carbohydrate coverage is its inflexibility, as patients must eat around the same number of carbs for all meals of the day. Too many or too few carbs for this dose could lead to hyper- or hypoglycemia respectively.
Insulin to Carbohydrate Ratio (I:C) Method:
The insulin to carbohydrate ratio method involves a mathematical calculation to determine the amount of rapid-acting insulin needed for coverage of the anticipated carbohydrates to be eaten at a given meal.
I:C ratio of 1:10 means 1 unit of rapid-acting insulin will theoretically cover 10 grams (g) carbohydrates (CHO).
Example B: Using I:C ratio to determine the amount of rapid-acting insulin for a meal
- A patient uses an I:C of 1:25 for Breakfast and anticipates they will be eating a bowl of cereal with milk at breakfast consisting of a total of 42g of carbs (12g from 8oz of milk and 30g from 1/2 cup of cereal). How much rapid-acting insulin is needed for carbohydrate coverage for this patient’s breakfast?
- 42 grams of carbs for breakfast using a 1:25 ratio
- Units of insulin for carb coverage =42g /25g per 1 unit of insulin
- = 1.7 units of rapid-acting insulin needed to cover 42 g of carbs for breakfast
- Round to nearest 1/2 unit increment = 1.5 units
- A patient uses an I:C of 1:5 for Dinner and anticipates they will be eating a total of 62g of carbohydrate at dinner. How much insulin is needed for carbohydrate coverage for this patient’s dinner?
- 62 g of cab for dinner using a 1:5 ratio
- Units of insulin for carb coverage = 62g / 5g per 1 unit of insulin
- =12.4 units of rapid-acting insulin needed to cover 62g of carbs for dinner
- Round to nearest 1/2 unit increment = 12.5 units
Note: I:C ratios are inversely proportional to their strength. In other words, a smaller ratio (e.g. 1:5) is stronger (i.e. provides more insulin per carb) than a larger ratio (e.g. 1:25, which provides less insulin per carb). This is important when adjusting the insulin to carbohydrate ratios for patients as discussed further in Unit 5.
I:C ratios can also give you an idea of how “insulin sensitive” patients are, as patients who require smaller ratios are generally more insulin resistant (requiring more insulin) than patients who use larger ratios.
The I:C ratio method is advantageous over the constant carb diet method, as it allows for increased flexibility for patients who may have a varied diet and eat varying amounts of carbohydrates with meals throughout the day.
The insulin to carbohydrate ratio itself can be determined in two ways:
1. The “500-rule”
Example C: Calculating I:C Ratio using the “500-Rule”
- For our 6-year-old in our prior example with TDD of 10.2 u/day, we want to calculate his I:C ratio using the 500-rule and find out how much insulin he needs for his Lunch consisting of an anticipated 35g of carbohydrates.
-
- Take 500 divided by the TDD
- 500/TDD = 1 unit of insulin for “X” grams (g) of carbohydrates (CHO)
- 500/10.2 = 49 –> means 1 unit of insulin theoretically covers 49g of carbohydrates = 1:49
- Round to 1:50 (as this makes the math easier!)
- To cover 35g of carbohydrates, the patient would need:
- 35g / 50g per 1 unit of insulin
- = 0.7 units of insulin. As this cannot be delivered accurately by a standard syringe or insulin pen:
- Round down to 0.5 units if the patient is going to be sedentary (e.g. most kids in the hospital setting)
- Round up to 1 unit if the patient is going to be active and running around
2. For our 14-year-old in our prior example with TDD of 44.3 u/day, we want to calculate her I:C ratio using the 500-rule and find out how much insulin she needs for her Dinner consisting of an anticipated 73g of carbohydrates.
-
- 500/TDD = 1 unit of insulin for “X” g of CHO
- 500/44.3 = 11.3 –> means 1 unit of insulin theoretically covers ~11g of carbohydrates = 1:11
- To cover 73 g of CHO for dinner, the patient would need:
- 73g / 11g per 1 unit of insulin
- = 6.6 units of insulin –> Rounded to 6.5 units which can be accurately delivered by insulin syringe or insulin pen
This method tends to be the most conservative calculation when determining the I:C for a patient with new-onset diabetes mellitus in that it usually leads to ratios that give <50% of the TDD as bolus insulin. This method is good to use in patients who are predicted to be very insulin sensitive.
2. Based on the constant carb calculation:
An I:C ratio can also be derived from the calculations used in the Constant Carb Method discussed above. However, this I:C ratio is generally stronger than the ratios derived from the 500-rule calculation. Therefore, I:C ratios using this method may increase the risk for iatrogenic hypoglycemia.
Neither method is incorrect, however, some faculty will prefer to use one method over the other. Others will calculate I:C ratios using both methods and use a ratio that “splits the difference”.
Example D: Calculating the I:C ratio from the Constant Carb Method
- Using our answer from Example B for our 6-year-old patient who we found needed 1.5 units of insulin per meal consisting of a target of 40-45g of carbohydrate (CHO) per meal on a Constant Carb Diet. What is this patient’s equivalent I:C ratio?
- As 1.5 units of rapid-acting insulin is used to cover 40-45g of CHO, we can see that:
- 40g CHO/1.5 units = 26.7
- 45g CHO/1.5 units = 30
- So this patient’s actual I:C ranges between 1 unit for every 25 g CHO (1:25) and 1 unit for every 30 g CHO (1:30).
- Compared to our I:C ratio calculated using the 500-rule in Example C (1:50), we see that these ratios derived from the Constant Carb Method are stronger.
- Thus, a conservative approach would be to “split the difference” and use a ratio of 1:35 or 1:40
- As 1.5 units of rapid-acting insulin is used to cover 40-45g of CHO, we can see that:
- Using our answer from Example B for our 14-year-old who we found needed 12.5 units of insulin per meal consisting of a target of 60-65 g of CHO per meal on a Constant Carb Diet. What is this patient’s equivalent I:C ratio?
- As 12.5 units of rapid-acting insulin is used to cover 60-65 g of CHO, we can see that:
- 60 g CHO/12.5 units = 4.8
- 65 g CHO/ 12.5 units = 5.2
- So this patient’s actual I:C is about 1 unit for every 5 grams of CHO (1:5)
- Compared to our I:C ratio calculated using the 500-rule in Example C (1:11), a ratio of 1:5 is 2 x stronger!
- Therefore, a conservative approach would be to “split the difference” and use a ratio of 1:8 or 1:9
- As 12.5 units of rapid-acting insulin is used to cover 60-65 g of CHO, we can see that:
Quiz Yourself:


Feedback/Errata