Calculating Total Daily Dose
For every patient admitted with new-onset diabetes mellitus, regardless of whether they present with DKA, they will eventually need to be started on an initial basal/bolus insulin regimen consisting of multiple daily injections (MDI therapy).
Figure 1 summarizes the basic steps needed to calculate such a regimen.
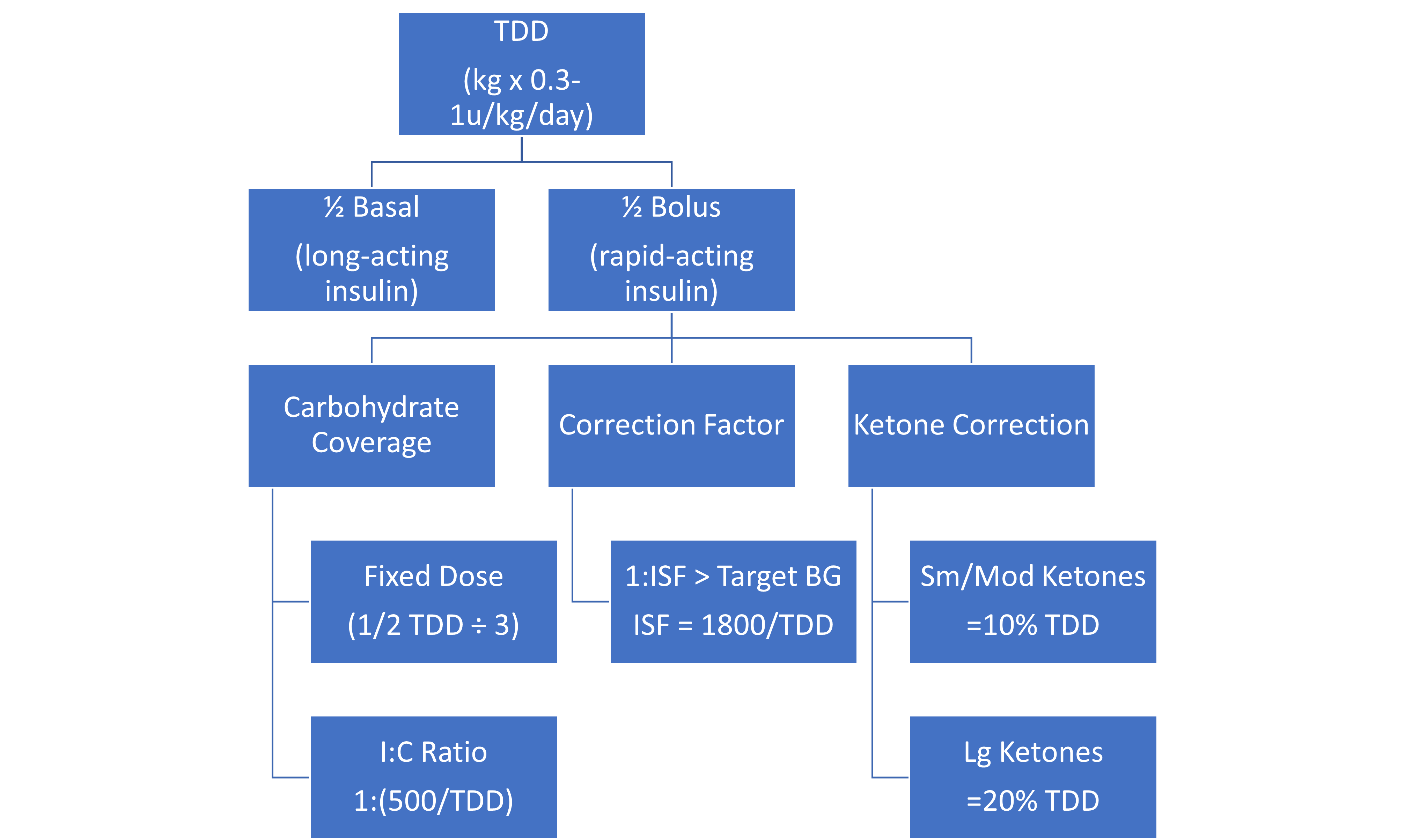
The remainder of this unit discusses the details and considerations that go into each of these calculations so that the regimen can be further optimized for the individual patient. Overall, the initial regimen is an “educated guess” with the goal of preventing excessive hypoglycemia and hyperglycemia.
Further adjustments are made to the individual components of the insulin regimen (e.g. the insulin-to-carbohydrate ratios, hyperglycemia correction, etc.) based on the evaluation of daily glucose trends in the outpatient setting. Hence, a new insulin regimen does not need to be “re-calculated” for patients with known diabetes who already have an established insulin regimen. Adjustments to the insulin regimen are discussed further in Unit 5.
The first step in calculating the insulin regimen is determining how to calculate the total daily dose (TDD). TDD represents the total amount of daily insulin (basal and bolus insulin) needed by an individual during a 24-hour period.
This initial calculation is an educated guess guided by various factors used to estimate how “insulin sensitive” a patient will be. These factors include:
- Patient age
- Weight
- Stage of puberty
- The severity of the patient’s initial presentation
In general, a young, non-obese, pre-pubertal child will be more insulin sensitive than an older, obese, pubertal child.
For children, initial TDD is calculated based on a range of 0.5 units/kg/day to 1 unit/kg/day.
Each endocrinologist may arrive at a slightly different initial TDD for each patient; however, the following algorithm in Figure 2 can help guide your decision about where to start on this TDD spectrum:

Some physicians will also consider the severity of the patient’s diabetes presentation. For example, a patient who does not present in DKA and has a lower HbA1c (<9-10%) is likely more insulin sensitive when compared to a patient who presents in DKA or has a more elevated HbA1c. This is because the later patient is likely to have more significant glucotoxicity causing their remaining functional beta-cells to be “stunned” and unable to produce endogenous insulin.
This glucotoxicity resolves when glucose levels are maintained in a more normal range, and the remaining functional beta-cells “wake up” and start reproducing endogenous insulin. This leads to a period of time, called “the honeymoon period” during which patients rely on less exogenous insulin to maintain normal blood glucose (Figure 3).
As the autoimmune process in Type 1 diabetes continues, this remaining functional beta-cell mass eventually succumbs to autoimmune destruction and the patient’s insulin requirements increase. The honeymoon period is variable and unpredictable from one patient to the next, and may last weeks, months, or even up to a few years.

Once you have determined where your patient falls on the TDD spectrum, use your selected total daily dose and multiply by the patient’s weight to determine the total number of units of insulin the patient needs in a 24-hour period.
Examples: Calculating TDD for new-onset T1DM MDI Basal/Bolus Insulin Regimen
- A 6-year-old, non-obese (17kg), prepubertal male presents in moderate DKA with an initial HbA1c of 11%.
- If we use the algorithm in Figure 2 we find TDD range should be 0.5-0.6 u/kg/day
- As he is presenting in DKA and has HbA1c >10%, we will assume he is a bit more insulin resistant, so we will use the upper end of this range, thus TDD of 0.6 u/kg/day
- TDD * weight (in kg) = total units of insulin per day
- 0.6 u/kg/day * 17 kg = 10.2 units/day
- A 14-year-old, non-obese (59 kg), pubertal female presents with hyperglycemia, HbA1c 9%, and has suspected T1DM based on second-tier laboratory testing.
- Using Figure 2, TDD range is 0.75-0.8 u/kg/day
- The patient is not presenting with DKA and does not have a very elevated HbA1c, so the lower end of this range is used.
- TDD * weight (in kg) = total units of insulin per day
- 0.75 u/kg/day * 59kg = 44.3 units/day
It is also important to know how to determine an average TDD for patients with known DM who are already on insulin, as this is often used to determine how much rapid-acting insulin is needed for the ketone corrections.
In these cases, TDD is determined by adding up all of the rapid-acting insulin from mealtime doses and the long-acting insulin doses taken over an average 24-hour period.
Example: Calculating TDD for known T1D on MDI Therapy
1. Ask the patient to review, on average, the doses they take for a standard breakfast, lunch, and dinner. Add these together and include the long-acting insulin dose.
Breakfast dose: 8 units
Lunch dose: 5 units
Dinner dose: 7 units
Long-acting dose: 20 units
Total daily dose: 40 units
2. Alternatively, if you know the I:C ratios for meals and know approximately how many carbs they eat per meal, you can estimate TDD by calculating their meals doses and then adding the long-acting insulin dose.
Breakfast: I:C is 1:10, usually eating ~50g CHO = 5 units
Lunch: I:C is 1:15, usually eating 45g CHO = 3 units
Dinner: I:C is 1:8, usually eating 60g CHO = 7.5 units
Long-acting dose: 25 units
Total Daily Dose: 40.5 units
Average TDD is easy to find for patients who are on insulin pumps, as the pumps keep track of delivered insulin and will report an average TDD over the last 7 days (you can ask patients to find this in their pump settings).
Example: Finding TDD for known T1D on an Insulin Pump
The patient or family should be able to find this information on their own, however, if they cannot, you can use the following instructions to help them find this within their pump.
Quiz Yourself:
Recommended Additional Reading:
More comprehensive information about insulin treatment in Type 1 diabetes can be found at:
Cengiz E, Danne T, Ahmad T, Ayyavoo A, Beran D, Ehtisham S, Fairchild J, Jarosz-Chobot P, Ng SM, Paterson M, Codner E. ISPAD Clinical Practice Consensus Guidelines 2022: Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes. 2022 Dec;23(8):1277-1296. doi: 10.1111/pedi.13442. PMID: 36537533.


Feedback/Errata