3 Craniospinal Irradiation (CSI)
Patient Simulation: Craniospinal Irradiation (CSI)
Medulloblastomas are a type of pediatric primary brain tumor accounting for approximately 20% of primary pediatric brain tumors. These tumors originate from primitive neuroepithelial tissues (PNET) and are classified as high-grade gliomas. They tend to spread via the cerebrospinal fluid (CSF) necessitating craniospinal irradiation. Oligodendrogliomas and Ependymomas can also spread through the CSF which may necessitate CSI.
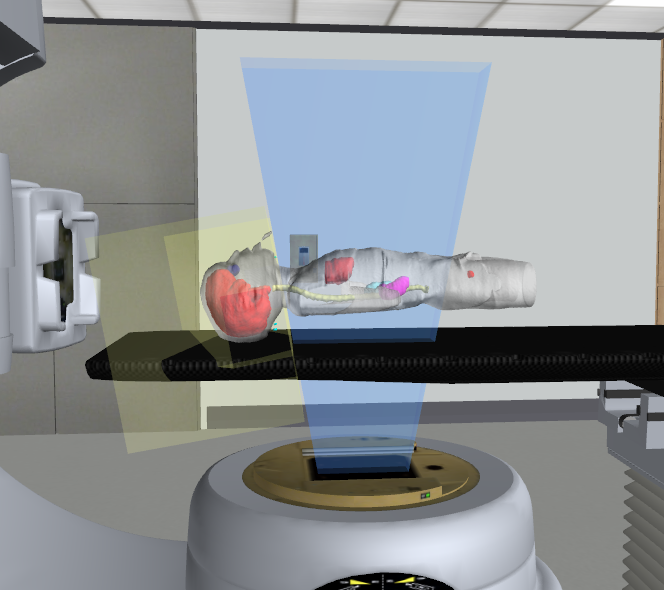
Historically, patients were simulated and treated in the prone position to visualize the spine and gap between spinal fields (if more than one). For conventional simulation, the spine field is simulated first to obtain the collimator angle for the brain fields relative to the length of the spine field. Due to advances in imaging and treatment technology, most patients today are positioned supine. The supine position is more comfortable and reproducible; it also allows for access to the patient’s airway if anesthesia is required.
Ensure the patient is positioned straight with their arms are at their side. Use a thermoplastic head and shoulder mask for head, neck, and upper spine alignment. A vacloc can be used under the lower extremities for pelvis and low spine alignment. If the patient is a small child, a body vacloc could be used abutting the headrest and a brain mask. Custom headrests can also improve comfort and reproducibility. Localization marks should be placed on the lateral and anterior aspects of the brain field with straightening marks down the abdomen for reproducibility of the spine position and lateral leveling marks for rotation. The simulation scan should extend from the patient’s vertex through the sacrum.
Treatment Volume Localization: CSI
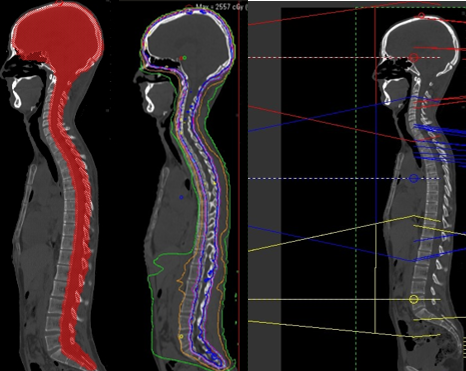
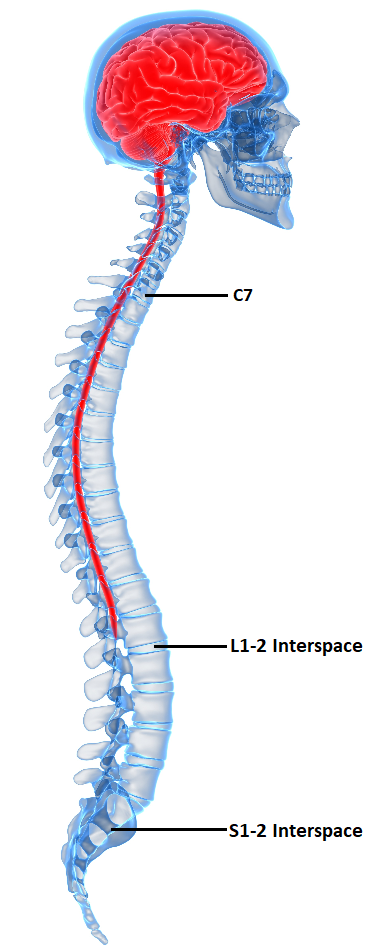
Craniospinal Irradiation (CSI) treats all parts of the cranial and spinal cavities where CSF flows, terminating at the second sacral vertebrae. The cranial field boarders are the same as the whole brain fields apart from the inferior border extending from mastoid tip to approximately C5-7 to include the cervical spinal cord with a 2 cm margin. Treating the cervical portion of the spine with the lateral brain fields is advantageous to block the structures anterior to the spine that would otherwise receive exit dose from the posterior spine field. Additionally, a lower superior boarder of the posterior spine field will reduce divergence towards the patients mandible. The spine field will use an abutting or feathering technique and will extend to approximately S2. A feathering technique uses the MLCs to blend the dose at field junctions to avoid overdosing the spinal cord. Similarly, IMRT treatment techniques can blend the dose between fields. See Figure above.
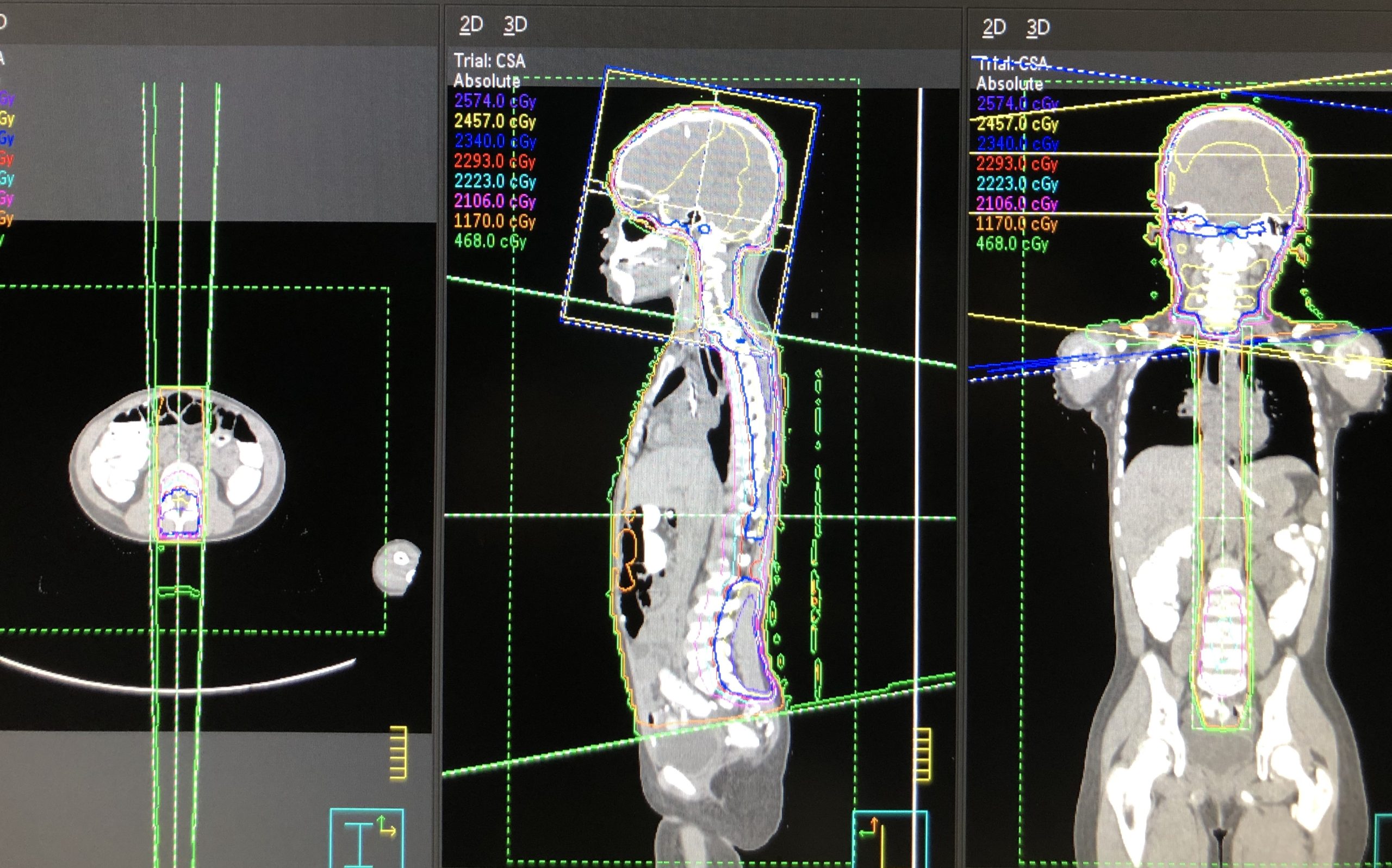
Historically, treatment consisted of lateral brain fields and posterior spine field(s). Careful planning and consideration must be given to match lines between the inferior aspect of the cranial field and superior aspect of the spinal field. The spinal field can be delivered at an extended distance to accommodate the entire spine length in one field or delivered in two fields utilizing a gap calculation or feathering to prevent overdosing the spinal cord at the field match.

If the plan necessitates more than one spine field, and fields are static, the field gap must be calculated. The gap measures the separation of the two fields on the patient’s skin’s surface; this ensures field overlap occurs at a depth anterior to the spinal cord. All matching measurements, including the cervical spine field, are easiest with the patient in the prone position with this treatment technique. The lateral brain fields need superior flash that extends beyond the vertex by several cm to support the shifting of fields and match lines by .5-1 cm approximately 2-3 times during treatment.
Field matching: Couch and collimator rotations are needed for 3D plans to prevent beam overlap and the potential devastating effects of a spinal cord overdose. The inferior border of the lateral cranial fields will overlap with superior border of the posterior spine field; the two divergences need to be accounted for. The cephalad aspect of the spine field diverges towards the cranial field, to account for this divergence, match the collimator rotation of the cranial field to the divergence of the spine field.
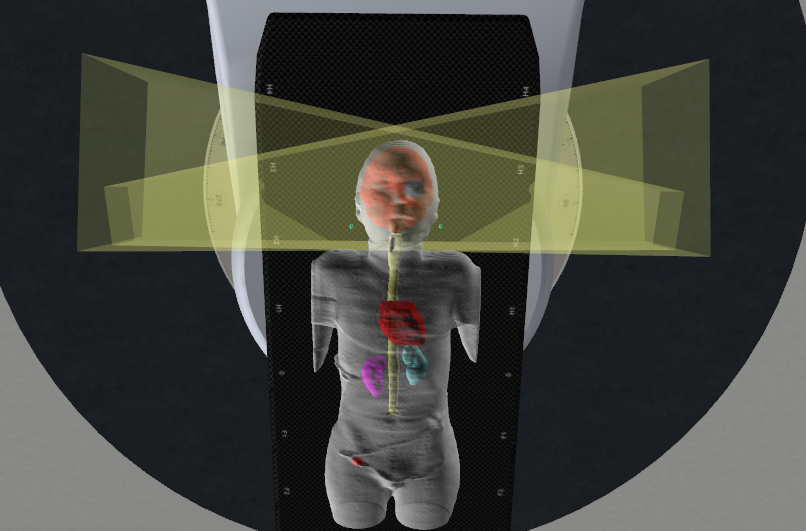
The second divergence involves the inferior aspect of the cranial fields diverging into the spinal field, rotate the foot of the couch toward the gantry until the inferior border of the cranial field is parallel or matched the superior aspect of the spinal field. The couch angle depends on the length of the lateral brain fields, approximately 5 degrees. When foot of couch rotates toward collimator, treatment distance in inferior half of brain field decreases, increasing dose. The superior portion of the field, the distance increases and dose decreases. The couch rotation can also lead to the most inferior aspect of the opposite temporal fossa to be missed.
Treatment Techniques: CSI
Emerging Technologies & Treatments: CSI
- TomoTherapy offers possibility of irradiating large target volumes continuously and homogeneously without gapes and junctions. This ensures irradiation of entire neuroaxis in one session, short treatment times, and a full 360-degree treatment. Elective dose reduction to OARs and direct image verification of patient position via CT.
- Protons improve normal tissue sparing while also providing more homogenous target coverage than photons. Lower risk of secondary cancer and non-cancer adverse effects.
- IMRT/VMAT delivery techniques continue to make advancements in field-matching techniques.
Media Attributions
- medically accurate 3d rendering of a human brain and spine © SciePro adapted by Jared Stiles is licensed under a All Rights Reserved license
- 3 isocenter VMAT CSI plan © University of Iowa Hospitals and Clinics Radiation Therapy Program is licensed under a CC BY (Attribution) license
- 3D conformal CSI treatment plan © University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Sagittal isodose line distribution for a photon CSI © Vertual Ltd is licensed under a All Rights Reserved license
- CSI spine divergence © Vertual Ltd is licensed under a All Rights Reserved license
- Brain filed divergence © Vertual Ltd is licensed under a All Rights Reserved license
fixed; do not change in shape or intensity

