11 Salivary Glands
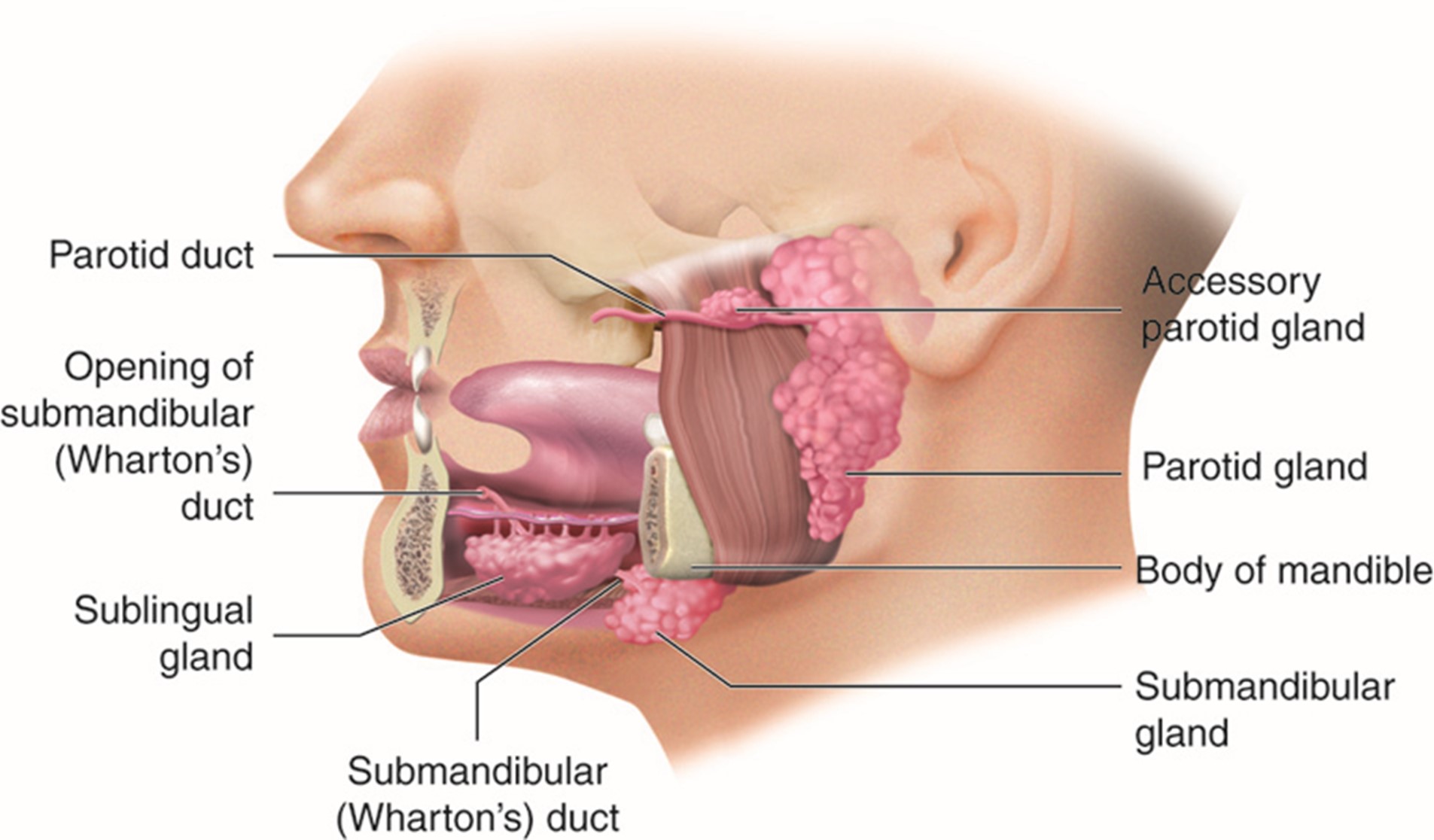
The salivary glands consist of two major groups, the major and minor salivary glands. The major glands are the Parotid, Submandibular, and Sublingual glands. The word parotid means around the ear. The parotid gland is shaped by the structures that surround it. Superiorly the border lies below the zygomatic arch and below the external auditory meatus (EAM). Posteriorly it extends to the tip of the mastoid. Anteriorly the gland extends to the orifice of the parotid duct. Inferiorly the gland extends to the upper border of the posterior belly of the digastric muscle. Radiographically this lies between the mandible and the hyoid. The minor salivary glands are the labial and buccal glands, the gloss palatine, palatine, and lingual glands. These glands are commonly named after structures that they are adjacent to. You can visualize all the glands in the following diagrams.
The American cancer society states that there will be roughly 2500 new cases of malignant salivary cancer each year, representing approximately 7% of all head and neck cancers. The primary histology of these glandular structures is adenocarcinoma. Most cancers are located in the largest salivary glands, the parotids. Malignant disease is most significant in the parotid glands because of the high incidence of tumors, even though two-thirds of tumors will be benign. The minor salivary glands will have a higher rate of malignant disease; roughly 75% will be malignant. The histologic breakdown of adenocarcinomas will commonly be adenoid cystic and mucoepidermoid disease. Of the pathologies, Mucoepidermoid disease is more common, and adenoid cystic carcinomas will generally have worse outcomes, therefore, the treatment should be more aggressive.
Patient Simulation & Special Considerations: Salivary Glands
Simulation for salivary gland cancers will be similar to other head and neck cancers. Please refer to the “Patient Simulation: H&N” section.
When treating salivary gland malignancies, it is important to include the postoperative scar, which must be considered while making the thermoplastic mask. Triangulation localization marks are generally placed on the chin anteriorly and inferior to the EAM on both sides. When obtaining the topogram, the therapist will set the scan borders from the vertex to the hyoid bone. If cervical nodes are involved, the inferior board may be extended below the clavicles to the carina.
Treatment Volume Localization: Salivary Glands
There are multiple special considerations when planning radiation treatments for salivary gland cancer. It is crucial to understand how salivary cancers spread. The superficial lymph nodes of the parotid receive drainage from the subcutaneous tissue of the face, auricle, middle ear, and external auditory canal. Due to this drainage, the parotid is commonly involved with metastatic diseases and primary parotid tumors. Most malignant tumors spread through local invasion, ipsilateral neck lymph node spread, and perineural invasion. One-quarter of parotid tumors present with lymph node metastases, and another quarter have facial nerve palsy from the invasion of cranial nerve seven. The primary route of lymph node spread will continue to the first echelon of drainage, the ipsilateral jugulodigastric lymph node.
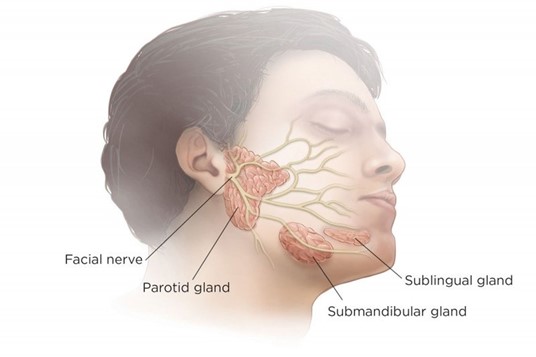
Cranial nerve involvement is likely for patients with bulky disease in the major salivary glands. The facial nerve (VII) has extensive bifurcation through the parotid, submandibular and sublingual glands. An increase in pressure on this nerve can lead to Bell’s Palsy; this leaves the facial muscles in a state of paralysis. This condition is accompanied by pain and discomfort on the involved side of the face. Other symptoms include slurred speech, difficulty opening and closing the eyelid, and dysphagia.
The salivary glands are very radiosensitive and are commonly spared, so it is important to avoid the contralateral gland when treating parotid gland disease. These glands are vital in producing saliva, aiding mastication, and preventing tooth decay. It is crucial to ensure that the dose falloff from treating the involved gland is rapid enough to avoid xerostomia in the contralateral side.
Historically, conformal treatment techniques use two or three ipsilateral photon beams to provide a homogenous dose distribution to the CTV without exceeding the tolerance of the adjacent critical structures. The three-field technique uses a lateral beam and anterior and posterior oblique fields with wedges. A single mixed photon and electron beam may also be used as the primary treatment technique. If this is done, the field should include the entire incision and the parotid bed with a margin. The dose should be prescribed beyond the deepest lobe of the parotid gland, approximately 4 cm.
-
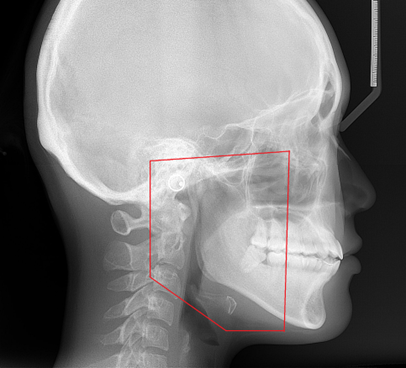
General treatment borders for a parotid gland. Superior: zygomatic arch
- Inferior: top of thyroid cartilage
- Posterior: behind the mastoid process
- Anterior: anterior to the border of the masseter muscle
Treatments today still follow these general borders but are more conformal to targeted tissues, sparing normal tissues and reducing toxicity. Please refer to the “Treatment Volume Location: H&N” section.
Treatment Techniques: Salivary Glands
Treatment doses for salivary glands are highly dependent on the stage of the disease. Surgery to remove either a section of or the entire parotid gland is likely the treatment of choice for stage 1 and 2 diseases. Radiation therapy may be recommended for positive margins or residual disease. If there are clear margins, the optimal dose will be approximately 60 Gy following standard fractionation. If there is evidence of residual disease, the total dose is increased by approximately 10 Gy to a total dose range of 70-75 Gy.
Advanced-stage diseases, stages 3 and 4, will result in a much more challenging surgical resection due to the vast amount of cervical lymph nodes involved. Surgery is possible but is generally not recommended. At this stage, with the progression of the disease, it is more likely that systemic chemotherapy will be combined with radiation to a dose of 70-75 Gy. Because salivary gland tumors are so rare, these patients are good candidates for further clinical trials to investigate disease treatment. Treatment margins for IMRT are reflected in the “Treatment Techniques: H&N” section.
Media Attributions
- Salivary gland locations © Cenveo is licensed under a CC BY (Attribution) license
- An Overview Of Parotid Glands © Juan Reddish is licensed under a CC BY-SA (Attribution ShareAlike) license
- Cephalometric radiograph © ANUG adapted by Jared Stiles is licensed under a CC BY-SA (Attribution ShareAlike) license
Refers to the other side (of the body)

