8 Oropharynx
Overview: Oropharynx
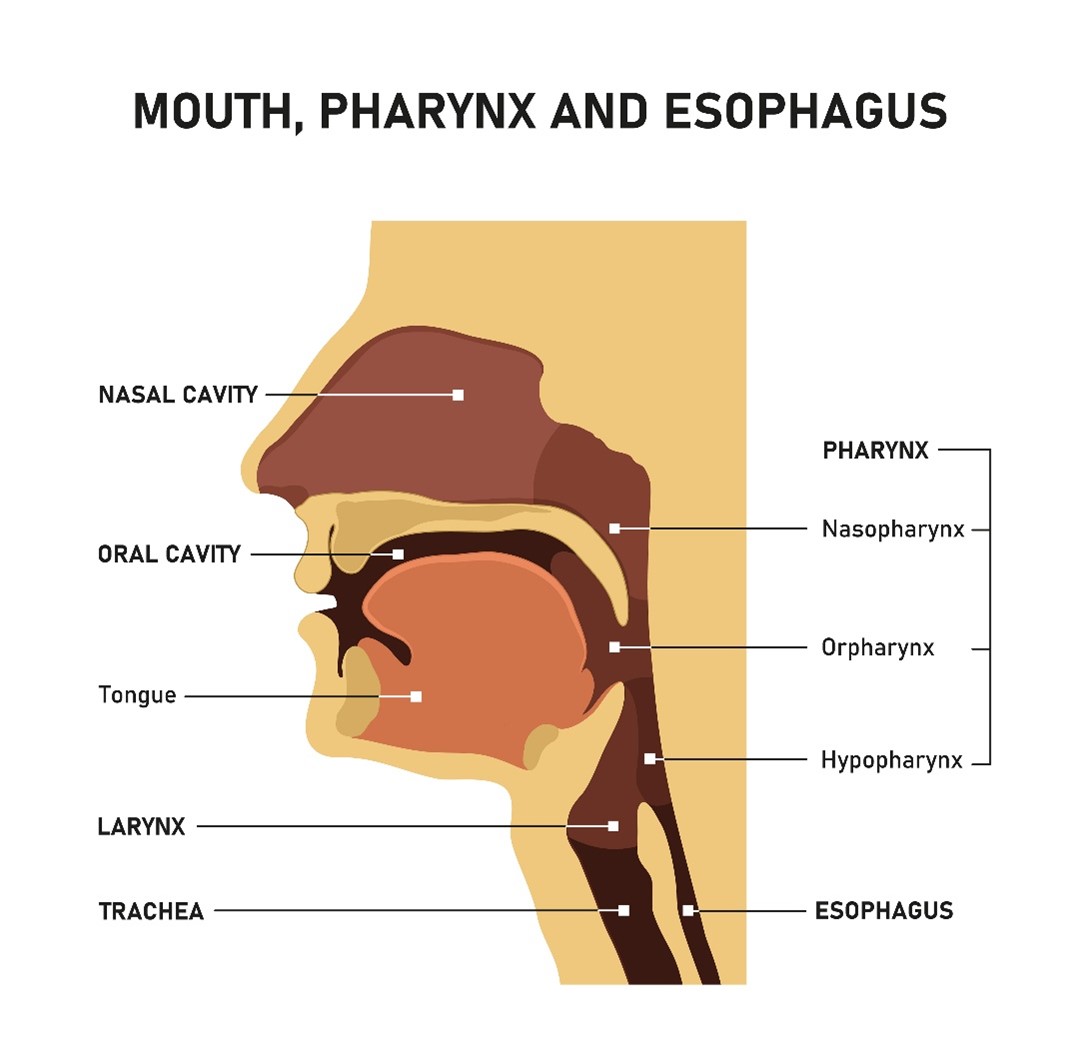
Oropharynx tumors are close to the oral cavity but lie more posteriorly. The general rule of thumb is that head and neck cancers have a poorer prognosis as the affected site moves posterior from the lips and inferiorly. Oropharyngeal cancers typically arise as squamous cell carcinomas (95%). Lymphoma and lymphoepithelial tumors are rare but can occur. Tonsils are the most common primary site of disease within this group. Common symptoms at clinical presentation are sore throat and painful swallowing. Tumors in this region have a profound effect on aerodigestive function.
The anatomical position of the oropharynx makes surgical intervention more difficult; most tumors are inoperable. The primary treatment option is radiation therapy. Radiation therapy is the treatment of choice for early-stage oropharyngeal tumors. Large extensive tumors are commonly treated with combined surgery and postoperative radiation. Radiation therapy alone is often used for inoperable patients and palliation.
Patient Simulation: Oropharynx
The simulation process is consistent with the typical head and neck in treating oropharynx lesions. Please refer to the “Patient Simulation: H&N” section. An additional consideration is the potential necessity of tongue immobilization. Depending on the anatomic location of the disease, it may be beneficial to depress the tongue into the floor of the mouth – this will reduce variability in tissue location and help spare normal tissues. The base of tongue cancer could be an example where the tongue would be immobilized to the floor of the mouth. The opposite technique may also be helpful – if treatment is of the lateral pharyngeal wall, the tongue may be immobilized away from the floor of the mouth.
Oral positioning video from “Simulation: Oral Cavity.”
Treatment Volume Localization: Oropharynx
- Anterior: 2 cm anterior to the tumor
- Posterior: behind the spinous process to include the posterior cervical lymph node chain
- Superior: entire jugular chain and above C1
- Inferior: thyroid notch, or to include the supraclavicular region
Treatments today still follow these general borders but are more conformal to targeted tissues, sparing normal tissues and reducing toxicity. The treatment planning is consistent with the typical head and neck protocol in treating oropharynx cancers. Please refer to the “Treatment Volume Location: H&N” section.
Historical treatments included a separate anterior lower neck field, “yoke field,” to treat the supraclavicular and lower jugular lymph nodes. Treatment of these nodes is crucial due to bilateral lymph node involvement. The yoke field abuts opposed laterals. The field match is most easily achieved using a half-beam block and a single isocenter, but a two-isocenter technique can be used with a couch-kick and collimator rotation for beam matching.
Different sites within the oropharynx have unique lymph node drainage pathways to consider in treatment planning.
| Oropharynx Site | Lymph Node Drainage Pathway |
| Tonsil | Jugulodigastric & submaxillary nodes |
| Base of Tongue | Jugulodigastric, low cervical, & retropharyngeal nodes |
| Lateral Pharyngeal Wall | Retropharyngeal, pharyngeal, & jugulodigastric nodes |
| Soft Palate & Uvula | Jugulodigastric, submaxillary, & spinal accessory nodes |
Treatment Techniques: Oropharynx
Curative dose-fractionation schemes can vary depending on the intent of treatment. 70 Gy in 35 fractions would be a typical regiment for early-stage conventional treatment. A hypo-fractionated course may also be considered for patients who cannot complete as many treatments as the conventional dose.
Hypo-fractionated dose examples of the oropharynx include:
- 55 Gy in 20 fractions at 2.75 Gy per fraction
- 44 Gy in 22 daily fractions at 2 Gy per fraction
Palliative dose examples include:
- 30 Gy in 5 fractions of 6 Gy twice weekly for two and a half weeks or
- 20 Gy in 5 daily fractions of 4 Gy.
Most recently, VMAT treatments allow multiple arcs to simultaneously treat the cervical nodes and the primary tumor using margins reflected in “Treatment Techniques: H&N” section. However, it is beneficial to understand conventional treatment techniques and borders.
Media Attributions
- Picture15 © Adobe stock: 310857854

