20 Stomach, Liver, & Colon
Overview: Stomach, liver, & Colon
The stomach is a reservoir for food and aids in digestion after food enters from the esophagus. Distally, it connects to the small intestine at the duodenum. Cancers of the stomach typically grow slowly and develop over many years. Most cancers are classified and adenocarcinomas.
The liver is the largest solid organ in the body, located in the upper right quadrant of the abdomen. The most common type of primary liver cancer is hepatocellular carcinoma. Most tumors of the liver are secondary or metastasis from other sites. The common cancers that spread to the liver are from the pancreas, colon, rectum, breast, and lung. The gallbladder is surrounded by the liver and aids in the digestion of fatty foods. Cancers here are rare and most are adenocarcinomas.
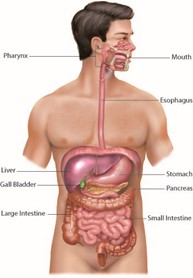
The colon (large bowel) consists of eight regions: the cecum, ascending colon, descending colon, splenic flexure, hepatic flexure, transverse colon, sigmoid, and rectum. The cecum, transverse colon, and sigmoid sections are located intraperitoneally and can be surgically removed unless the tumor is invading adjacent structures. The ascending colon, descending colon, hepatic flexures, and splenic flexures are located retroperitoneally or outside the peritoneum. Due to their location and lack of mesenteric support, cancers found in these portions of the colon commonly spread outside the bowel wall to adjacent soft tissues, like the kidney and pancreas. Lymphatic drainage along the colon is extremely rich and dependent upon the section of the colon. Most colon cancers are adenocarcinomas.
Patient simulation & Special Considerations: Stomach, liver, & Colon
The simulation process is consistent with the typical abdomen in treating cancers of the stomach, liver, and colon. Please refer to the Patient Simulation: Abdomen section. The stomach and colon are highly moveable structures and can shift locations depending on their fullness or emptiness. The physician may request patients may be NPO before simulation (also required if receiving contrast) and treatment. These structures may also benefit from motion management, like compression or 4D treatment, caused by respiration.
Stomach: When simulating a patient with stomach cancer, the doctor will want the patient to be NPO for up to 4 hours before treatment to keep the treatment volume smaller and consistent throughout treatment. It is essential to communicate these instructions with the patient.
Liver & Gallbladder: Some options for motion management include 4DCT, breath hold, gated breathing, fiducial tracking, abdominal compression, and MRgRT. Another vital aspect of simulation for liver treatment is that CT contrast is highly recommended. If a patient has any contraindications to IV contrast, fusing the image with an MRI for planning purposes is ideal.
Colon: Patient simulation for the abdominal colon will utilize a supine position with arms positioned high on the chest. One to two pillows should be situated under the patient’s head, and a lower vaclok used to immobilize the patient’s legs. The patient can also be simulated in a prone position, but this is usually reserved for malignancies of the distal (sigmoid) colon and rectum. Positioning the patient prone displaces the small bowel out of the pelvis. For more information about prone positioning, see the Special Simulation Considerations: Pelvis unit.
Treatment Volume Localization: Stomach, liver, & Colon
Stomach: Oral contrast at simulation will define the stomach. Regional lymph nodes at risk for disease include the pancreaticoduodenal, porta hepatis, supra-pancreatic, splenic hilar, and those of the greater and lesser curvature. The margins used in this structure’s treatment are variable; ideally, the stomach is empty and the entire volume is treated. The proximity of the heart can create challenges in treatment field design.
Liver & Gallbladder: A significant dose-limiting factor when treating the liver is radiation-induced hepatitis. However, this can be overcome with complex treatment plans and stereotactic treatments. Motion management is highly recommended for these treatments due to the diaphragm’s proximity. If this is not possible for the patient, then larger expansion volumes should be used to cover any uncertainties in the plan. When we are treating the gallbladder, we treat any involved nodes. This is often the common bile duct and hepatoduodenal ligament. The GTV is determined after the CT scan. The CTV should include the gallbladder fossa and adjacent liver and regional lymph nodes. Margins should be 20 mm craniocaudally and 8 mm anteroposterior, and 9 mm laterally to allow for breathing motion. Another option to compensate for breathing motion is gated treatment delivery.
Colon: The goal of treatment, whether preoperative or postoperative, is to include the primary tumor, or tumor bed, with a 4-5 cm margin. The primary nodal drainage pathways are typically included in the treatment fields.
|
Parts of colon
|
Lymphatic Drainage
|
|
Right colon
|
Follows superior mesenteric vessels and includes the ileocolic and right colic nodes.
|
|
Left colon
|
Follows inferior mesenteric vessels and includes the regional nodes termed the mid-colic, inferior mesenteric, and left colic.
|
|
sigmoid
|
Drains into the inferior mesenteric system and includes nodes along the superior rectal, sigmoidal, and sigmoidal mesenteric vessels.
|
|
Upper rectum
|
Follows superior rectal vessels into the inferior mesenteric system.
|
|
Middle/Lower rectum
|
Lymphatic drainage along the middle rectal vessels with the primary nodal group comprising of the internal iliac nodes.
Other nodal groups at risk of rectal cancer are the perirectal, lateral sacral, and presacral nodes. Low rectal lesions that extend into the anal canal can drain into the inguinal nodes. |
Refer to Treatment Volume Localization: Abdomen section for TD 5/5’s.
Treatment Techniques: Stomach, liver, & Colon
Stomach: The role of radiation therapy in stomach cancers is typically used adjuvant to surgery and chemotherapy. The most common treatment options are 3D-CRT or IMRT. According to The World Journal of Gastroenterology’s article, the radiation dose for these treatments would be 60 Gy in 1.5-2.0 Gy fractions for unresectable gastric cancer. Another trial at the Mayo Clinic treated unresectable gastric cancer with or without 5-FU chemo during the first three days of radiation and treated with 35-37.5 Gy in 4-5 weeks.
Liver & Gallbladder: For liver metastasis, 20-30 Gy in 13-29 fractions is delivered to the whole organ to relieve painful hepatomegaly. Another option is 20-25 Gy to in 2-3 weeks. For lesions <5 cm, SBRT is the treatment of choice, giving 45-54 Gy in 3-5 fractions. For more information about SBRT treatments, review the Treatment Volume Localization: SBRT section.
The treatment regimen for gallbladder lesions is chemoradiation. This tends to have more potent side effects but is more effective, especially for nodal involvement. The gallbladder was historically treated with a field arrangement like a pancreatic tumor or through AP/PA fields. The target includes the primary lesion, adjacent tissues, and any involved regional nodes. The dose fractionation for inoperable gallbladder disease is 54 Gy in 20 fractions with a 15 Gy IORT boost. Another fractionation option is 35-55 Gy EBRT and 15 Gy in 3 fractions using brachytherapy.
Colon: The treatment of choice for rectal cancer is the surgical removal of the primary tumor and primary nodal drainage. Neoadjuvant Radiation Therapy, decreases the viability of tumor cells that could spread at the time of surgery, improving the ability to resect large tumors and reducing small bowel complications by radiating in a nonsurgical area. Adjuvant Radiation Therapy, has the advantage of better selection of patients for treatment based on the surgical and pathologic findings.
|
Treatment
|
Dose
|
|
Conventional (Curative)
|
45-50 Gy @ 1.8 – 2 Gy/fx (with a possible boost to follow)
|
|
Preoperative
|
Hypo-fractionated: 25 Gy in 5 fx
|
|
Boost:
|
Preoperative: 5.4 Gy @ 1.8 Gy/fx (50.4 Gy total)
Post-operative: 5.4 – 9 Gy @ 1.8 Gy/fx (50.4 – 61.2 Gy total) |
|
Palliative Radiation
|
Palliative chemoradiotherapy may be used for maximal local control of inoperable rectal cancers where prolonged survival is possible.
|
Emerging Technologies & Treatments: Stomach, liver, & Colon
Treatment advances and technologies available for the stomach, liver, and colon are the same as those described in the Emerging Technologies & Treatments: Abdomen section.
Media Attributions
- Major organs of the digestive system © Cenveo is licensed under a CC BY (Attribution) license
Intraperitoneal contents are within the thin, transparent peritoneum of the abdominal cavity containing the abdominal organs

