14 Stereotactic Body Radiation Therapy (SBRT)
Patient Simulation & Special Considerations: SBRT
To ensure the effectiveness of SBRT, it is crucial to immobilize the patient well and reproduce the setup precisely for each fraction. The dose per fraction is higher than conventional radiation therapy; this is possible because of the precise targeting and immobilization techniques used to minimize the radiation exposure to surrounding healthy tissues and organs. Patient positioning and treatment devices are used to reduce patient motion and increase treatment accuracy. The simulation process is consistent with the thorax simulation, but often, scans are 4D and use surface guidance because of the tight treatment margins. Please refer to the “Patient Simulation: Thorax” section.
Treatment Volume Localization: SBRT
SBRT is an advanced and precise technique for treating small and well-defined tumors. Treatments include tumors throughout the body, but common sites include the lungs and liver. It is commonly used for lung cancers in treating early-stage, non-small cell lung cancer. The treatment plan is designed in consideration of the tumor’s size, location, motion, and proximity to critical structures. Treatments deliver a concentrated and accurate dose of radiation to the tumor. Compared to traditional radiation therapy, SBRT offers the advantages of improved tumor control rates and reduced side effects. It achieves this by delivering high radiation doses in a small number of fractions, five or fewer.
The American Association of Physicists in Medicine (AAPM) Task Group 101 provides comprehensive guidelines on the use of SBRT for lung cancer. According to these guidelines, the maximum gross tumor volume (GTV) size for lung cancer treated with SBRT is typically limited to 5 cm. These guidelines evolve over time as new research and advancements in technology emerge. It is always recommended to consult with a radiation oncologist who can provide the most up-to-date and personalized information based on the specific clinical situation.
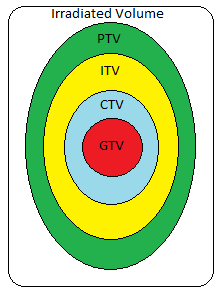
When designing the treatment volume for lung cancer, the physician identifies the visible extent of the disease, known as the gross tumor volume (GTV). A margin of 5-10mm is added to define the clinical target volume (CTV), which accounts for microscopic disease that may not be visible. Additionally, an internal target volume (ITV) is included to compensate for the internal movements of the CTV during treatment. Finally, the planning target volume (PTV) is determined by adding a margin to account for patient setup errors, encompassing both the CTV and internal margin. A common clinical practice is to avoid treating through the contralateral lung.
Treatment Techniques: SBRT
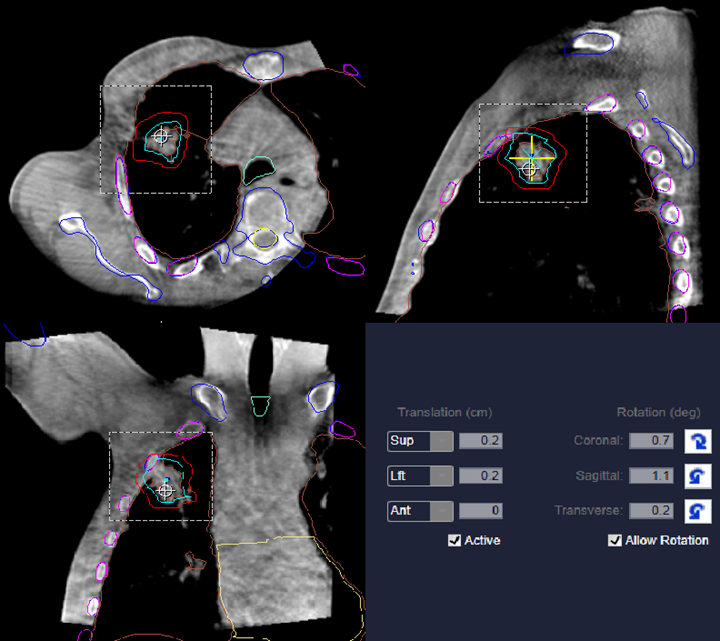
SBRT treatments often use 4D motion-monitoring systems to reduce uncertainties using IGRT as previously described. The specific protocol may vary between facilities, but image alignment and prescription verification from the oncologist and physicist is often required before administration due to the high dose per fraction. Treatments involve using multiple arcs or beams to precisely target the tumor, delivering a dose of 25-50 Gy in <5 fractions using standard energies of 6 and 10 MV. SBRT lung treatments should avoid critical structures and consists of various lateral, anterior, and posterior oblique beams.
The most common treatment technology used for SBRT treatments is a linac-based VMAT with CT or MRI image guidance. The flattening filter is often removed because of the small field size and to achieve a high-dose-rate – 1400 MU/minute; this reduces the length of treatment.
| SBRT | SRS | Standard Fractionation |
| Extracranial Treatments (outside the cranial cavity) | Intracranial Treatments (in the cranial cavity/brain) | Anywhere in the body |
| Tumor Size <5 cm | Tumor Size <3 cm | Any size treatment field, whole body to conformal |
| Hypofractionated (<5) | Single Fraction | Fractionated (~25 – 35) |
| High Doses, 6 – 30 Gy/fx; delivered 2-3 fx/wk (>40 hrs between fx) | High Doses (~18 – 90 Gy) | 1.8 – 2.0 Gy/fx; delivered M-F over 5-7 weeks |
Current research is comparing the use of a single isocenter versus multiple isocenters for SBRT treatments. In one study, a single isocenter approach for multiple lung metastases showed reduced treatment time and improved patient comfort, with a slight increase in lung dose as the trade-off. The authors suggest that this technique may be suitable for patients experiencing severe pain or with oligometastatic disease; it can also be highly beneficial for patients with multiple target volumes.
Other treatment technologies include the Accuray CyberKnife.
Media Attributions
- SBRT lung CBCT2.0 © University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Planning target volumes © Jared Stiles is licensed under a CC BY (Attribution) license
refers to the spread of cancer cells from the primary site to only one or two other parts of the body, resulting in new tumors

