27 Male Pelvis
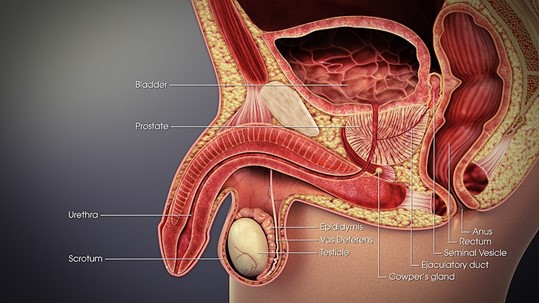
Overview: Male Pelvis
Prostate cancer is the most common cancer in men; approximately one in eight are diagnosed annually. The average age of diagnosis is sixty-six, and it is rare before the age of forty-four. In the US, where screening is standard, less than 5% of men have metastatic disease at presentation. The American Cancer Society recommends screening should begin at age 50 and includes a digital rectal exam and blood draw to review the PSA (Prostate Specific Antigen hormone). Other cancers of the male pelvis include penile and testicular cancer.
Overview: Prostate
The prostate is a walnut-shaped and sized gland. The function of the prostate is to produce fluid that supports the nourishment and transportation of sperm. It sits posterior and inferior to the bladder. The prostate also sits anterior to the rectum; this is a crucial detail to understand when localizing the prostate. The prostate’s location can shift based on the bladder and rectum’s fullness The urethra runs through the prostate, so dysfunction with the urinary stream is a common symptom of prostate cancer.
The pathology of prostate cancer is overwhelmingly adenocarcinoma. However, there are instances of squamous cell disease which are rare and aggressive. Etiological factors for prostate cancers include having a diet high in red meat. African American men have a one-and-a-half times higher risk than the general population. BRCA1 and 2 genetic mutations also increase a person’s risk of developing this disease over their lifetime.
The seminal vesicles are the most common site of direct local invasion. Lymphatic spread can also occur in the peri-prostatic nodes, followed by the obturator nodes. Further spread can be found in the internal iliac, external iliac, common iliac, and presacral nodes. Lastly, hematogenous metastases are seen with advanced-stage disease, commonly to the bone; these lesions can be osteoblastic.
Staging can be complex for prostate cancer; it is based on three key pieces of information: TNM, PSA, and Gleason score.
- TNM classification describes the extent of the primary tumor (T), the presence or absence of lymph node disease (N), and if the cancer has spread to other parts of the body (M).
- PSA (Prostate Specific Antigen) level is a measurement, a protein made by the cells in the prostate. Most men have a PSA level under 4ng/ML of blood, but this number rises with age with 10ng/ML still falling in normal limits. Conditions other than cancer can increase one’s PSA and no set cutoff point definitively informs you if a man does or does not have prostate cancer.
- Gleason score is a measure of the grade of prostate cancer. If the cell histology looks like normal prostate tissues, a grade of “1” is assigned. If the cancer looks very abnormal, a grade of “5” is assigned. Two different areas of the prostate are biopsied, and each is assigned a score. For example, if the Gleason score is written as 3+4, most of the tumor is grade 3, and less is grade 4. These numbers get added together to give a Gleason score of 7; the higher the score, the more aggressive the cancer.
Current recommendations for treating early-stage prostate cancers vary significantly due to their typically indolent nature. Treatment options include active surveillance, radical prostatectomy, radiation therapy, or Androgen Deprivation Therapy/hormone therapy. The patient’s age, health, stage of their disease, treatment side effects, and preference will help decide the best treatment course for each patient. For late-stage disease, more radical measures may take place; this may include an increased radiation dose, chemotherapy, and hormone treatment.
Patient Simulation & Special Considerations: Prostate
Prostate simulation is consistent with the general setup for pelvis patients. It is crucial to have the patient’s lower body immobilization to minimize intra-fraction motion. Commonly, patients will have a vaclok formed to their legs and a combination of pillows, blocks, or wedges to support their upper body. Patients should have a comfortably full bladder and empty rectum before the simulation. A full bladder will push small bowel out of the pelvis and the treatment area; an empty rectum will increase reproducibility daily.
Treatment Volume Localization: Prostate
Historically, a 3D conformal treatment technique known as a four-field box was the standard of care for radiotherapy to the prostate. The field borders depended on the stage of the disease, but in general, were:
- Superior: L4-5 to include the common iliac nodes
- Inferior: The inferior aspect of the ischial tuberosities which is about 1.5-2cm below the caudal aspect of the prostate
- Lateral: 1.5-2 cm beyond the lateral pelvic brim.
- Anterior: include the pubic symphysis.
- Posterior: transect the rectum
Treatments today still follow these general borders but are more conformal to targeted tissues, sparing normal tissues, and reducing toxicity. Please refer to the “Treatment Volume Location: Pelvis” section.
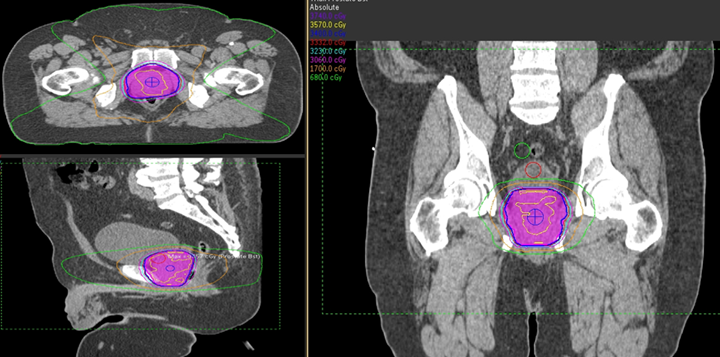
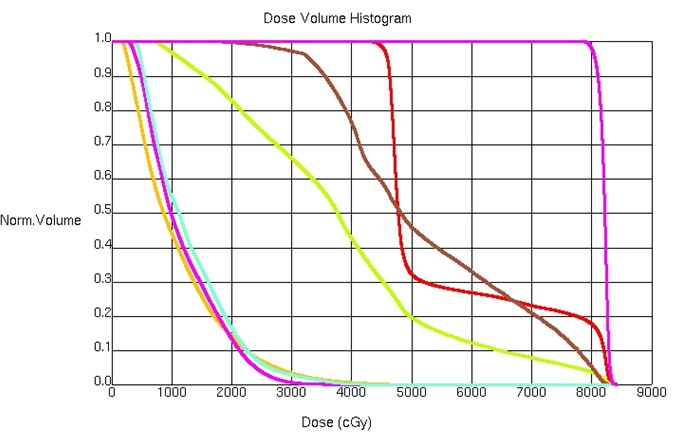
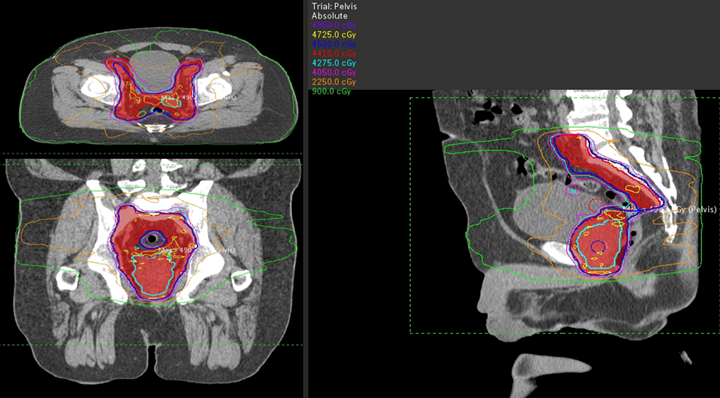
Treatment Techniques: Prostate
Radiation doses can vary significantly based on treatment delivery and patient risk profile.
External Beam:
- An external beam dose of 75.6-79.2 Gy at standard fractionation is recommended for low-risk patients.
- Intermediate and high-risk patients can receive doses up to 81 Gy to the prostate using standard fractionation. 45 Gy is delivered to the prostate, seminal vesicles, and nodes, while a simultaneous integrated boost to the prostate.
- Post-prostatectomy patients, a dose of 64-68Gy in standard fractionation is recommended for the prostate bed.
- A dose of 45-50 Gy to the prostate, seminal vesicles, and nodes is recommended when combined with a brachytherapy (HDR or LDR) boost to the prostate.
HDR:
HDR (High-Dose Rate) radiation therapy is a highly effective treatment option for prostate cancer. In this technique, a small, radioactive source, typically iridium-192, is temporarily placed inside or near the prostate gland using thin catheters. The source emits high-energy radiation for a short time, delivering precise and targeted doses to the cancerous cells. The advantage of HDR is that it allows for customized treatment plans, enabling doctors to adjust the dose distribution according to the tumor’s shape and location.
The total dose delivered during HDR radiation therapy to the prostate varies depending on the case. Two common HDR regimens for interstitial brachytherapy treatments use 18-20 catheters in one or two fraction treatments.
- For one fraction treatments, the prescribed dose is 15 Gy.
- For two fraction treatments, each fraction is 13.5 Gy to a total dose of 27 Gy, 1 week apart
It is common for the D90 (the minimum dose covering 90% of the volume) to receive a slightly higher dose than one hundred percent of the prescribed treatment dose between both fractionation schemes – the total is around 30 Gy. Additionally, the V100 (volume of the prostate that receives 100% of the prescribed dose) will commonly be in the range of ninety-five percent of the volume of the CTV.
Learn more about the HDR treatment procedure by watching: The High-Dose Rate (HDR) Brachytherapy Procedure to Treat Prostate Cancer
LDR:
LDR’s (Low Dose Rate) radiation therapy’s goal is to destroy cancer cells while minimizing damage to surrounding healthy tissues. It involves the use of permanently implanted radioactive sources “seeds” – typically, 50 to 125 of either iodine-125 or palladium-103. These seeds deliver a continuous low dose of radiation over a prolonged period until they are stable or no longer radioactive. The total dose of radiation delivered depends on several factors but is usually in the range of 150-200 Gy; this varies by case.
Watch this video review of treatment options and considerations in the treatment of prostate cancer: Prostate cancer: Brachytherapy’s fight for survival.
Overview: Penile
The penis has both reproductive and urinary purposes. It is comprised of erectile tissues, smooth muscle tissue, connective tissue, nervous tissue, and skin and epithelial tissues. Penile cancer is commonly squamous cell carcinoma (95%) and accounts for fewer than 1% of cancers in men. Risk factors include: being uncircumcised, HPV, tobacco use, immunosuppression, UV exposure, and age. The average age of diagnosis is 68 years.
Treatment for penile cancer depends on the type and stage of the cancer as well as the patient’s age and health. The primary treatment option for penile cancer is surgery but the size, location, and patient preference may limit its use. Sometimes radiation therapy may be used as the primary treatment or in addition to surgery. Chemotherapy is used for advanced cases or if the cancer has spread. The overall 5-year survival rate is 65%.
Patient Simulation & Special Considerations: Penile
The simulation process for penile cancer is consistent with the general setup for pelvis patients. However, when treating the penis, tissue reproducibility in the shape, size, and location is a unique challenge. Styrofoam molds and a custom bolus may be necessary to position, immobilize, and reproduce the position. Alternatively, patients can be positioned prone on a board to let the penis fall anteriorly into a water bath.
Treatment Volume Localization: Penile
Treatment volumes may include the primary tumor and/or inguinal and pelvic lymphatics to 50-60 Gy. A boost to the primary tumor of 5-10 Gy may be recommended. Bolus is required to bring the dose more superficial when using photon beams.
Treatment Techniques: Penile
Adaptive Radiotherapy (ART) can generate a treatment plan daily based on the size, shape, and location of the penis. Brachytherapy using a surface mold may be a desirable treatment technique for patients with penile cancer.
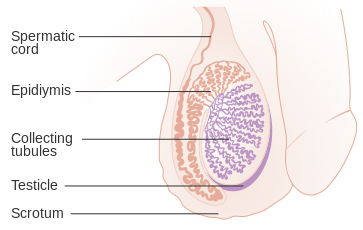
Overview: Testicular
Testicular cancer accounts for 1% of cancers in men, but it is the most common malignancy in males age 25-35. Men with a prior history of cryptorchidism have an increased risk. These cancers are most often detected by a palpable asymptomatic mass and are of germ cell histology (90%). These cells produce sperm and can be further classified as seminomas and non-seminomas – each with near equal incidence. These cancers can be further classified by cell-type. In general, testicular cancers have a good prognosis with about a 90% 5-year overall survival. For more information, consult cancer.org.
The management of these cancers can vary based on the pathology and stage. The standard of care for early-stage cancers is radical orchiectomy with a high ligation of the spermatic cord removed through an incision in the low anterior pelvis. Seminoma patients with residual disease are treated with chemotherapy or radiation, each has similar outcomes. However, chemotherapy is associated with less long-term toxicity and is preferred. Radiation therapy may be recommended based on the pathology or positive lymphatic disease after chemotherapy. Generally, seminomas respond well to radiation and are more likely to be treated with radiation than non-seminomas.
Patient Simulation & Special Considerations: Testicular
Simulation for testicular cancer is consistent with the general setup for pelvis patients. However, it’s important to position the patient’s hands high on their chest or above the head to account for the cephalic field-edge’s superior location. The treatment field is long; additional marks to level and straighten the patient are helpful.
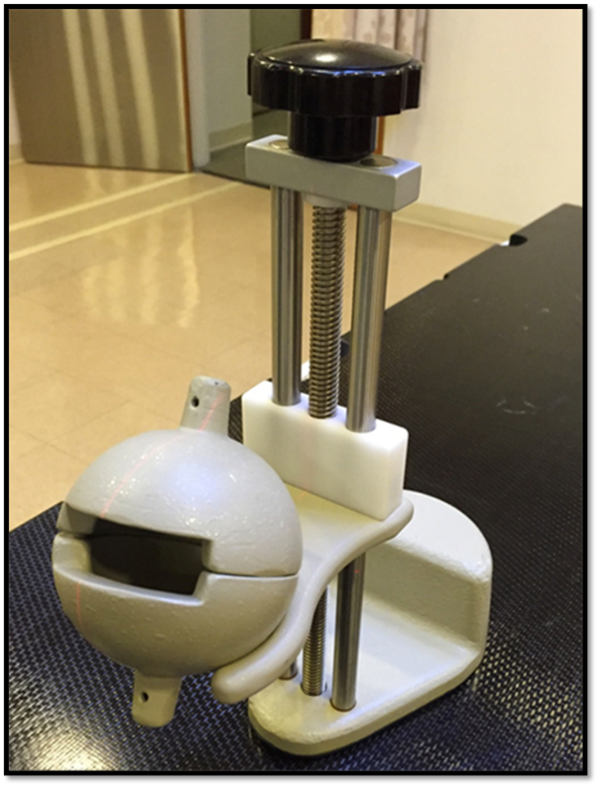
The patient may require the use of a testicular shield (clamshell) to protect the remaining testis and preserve fertility. Forming the base of the shield into the vaclok and frogging the patient’s legs is helpful for comfort and reproducibility. Warming the shield by running warm water over it or wrapping it in warm blankets makes it more comfortable for the patient and easier to relax the scrotum and tissues away from the body. Providing instruction on its use to the patient and protecting their modesty as much as possible by keeping them covered is best practice. Remember, part of the patient’s body is in the clamshell when attempting to position them. The typical scan parameters should extend from the dome of the diaphragm (T11) to the ischial tuberosities.
Treatment Volume Localization: Testicular
Historically, and often today, seminomas are treated AP/PA with a treatment field shape termed a “dogleg” or “hockey stick.” The first route of spread is to the periaortic lymph nodes; the treatment fields also include the ipsilateral renal hilar nodes, iliac nodes, and the surgical scar. Special attention must be given to the organs at risk, especially the kidneys. Treatment field borders are:
- Superior: Bottom of T11
- Inferior:
- Abdomen (Periaortic) portion: L5
- Pelvic portion: Pubic symphysis
- Lateral:
- Abdomen (Periaortic) portion: Transverse processes of vertebral bodies
- Pelvic portion: To include the ipsilateral common iliac and surgical scar
- Medial (Pelvis): Close to midline of the ipsilateral side
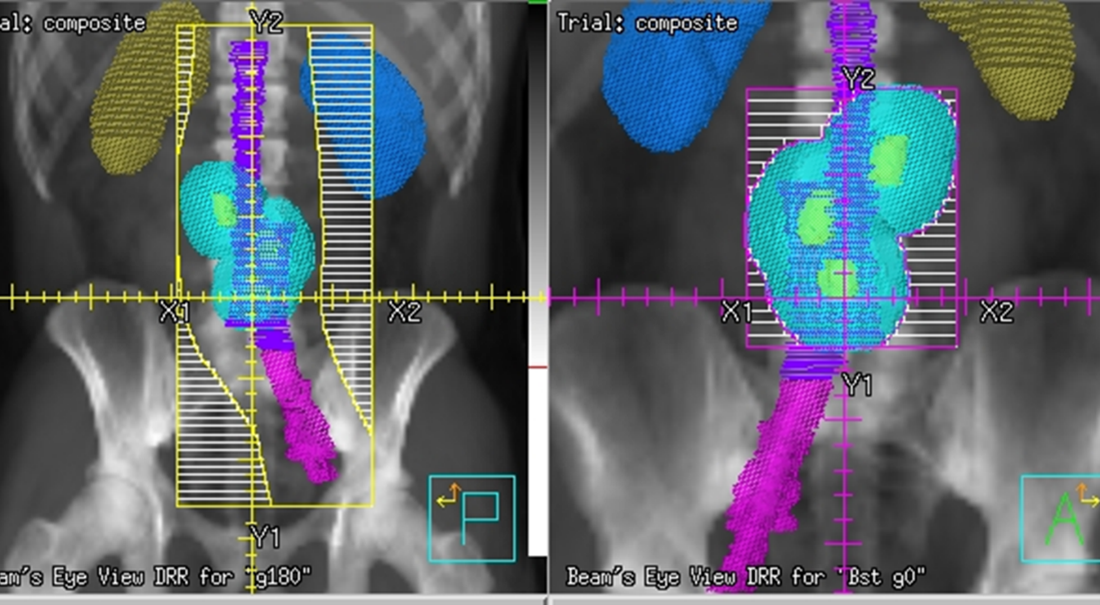
Due to the radiosensitivity of seminomas and the relatively low treatment dose required, traditional field borders remain common today. Treatment doses for the dogleg fields are around 20 Gy at 2 Gy per fraction. Smaller, more conformal, fields are treated AP/PA or using IMRT or VMAT technology to boost bulky disease and avoid critical structures to 30-36 Gy at 2 Gy per fraction.
Media Attributions
- 3D Medical Animation Vas Deferens © Scientific Animations is licensed under a CC BY-SA (Attribution ShareAlike) license
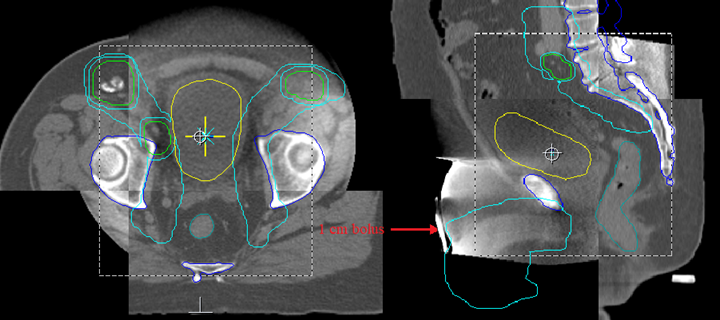
- VMAT plan of the prostate and pelvic nodes © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- VMAT boost to the prostate © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
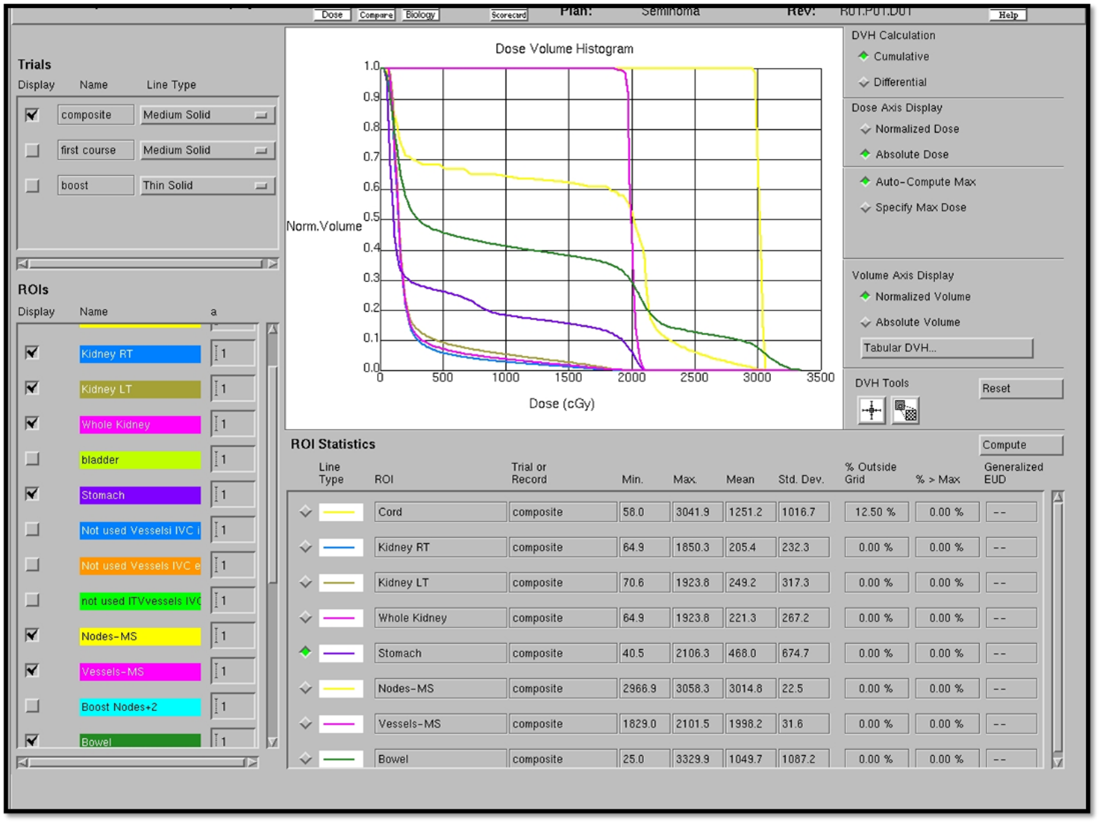
- DVH for a VMAT of the prostate © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Penile cancer cbct © The University of Iowa Radiation Therapy Program
- testis anatomy is licensed under a CC BY-SA (Attribution ShareAlike) license
- clamshell © The University of Iowa Radiation Therapy Program
- drrsdogleg © The University of Iowa Radiation Therapy Program
- dvhdogleg.pgn © The University of Iowa Radiation Therapy Program
A test done by a doctor that examines the lower rectum, posterior wall of the prostate, and anus
A protein produced in the prostate
Refers to forming new bone or osteoblasts and are commonly seen in prostate cancer
Hormone therapy for prostate cancer that reduces testosterone to prevent cancer cells from growing and spreading

