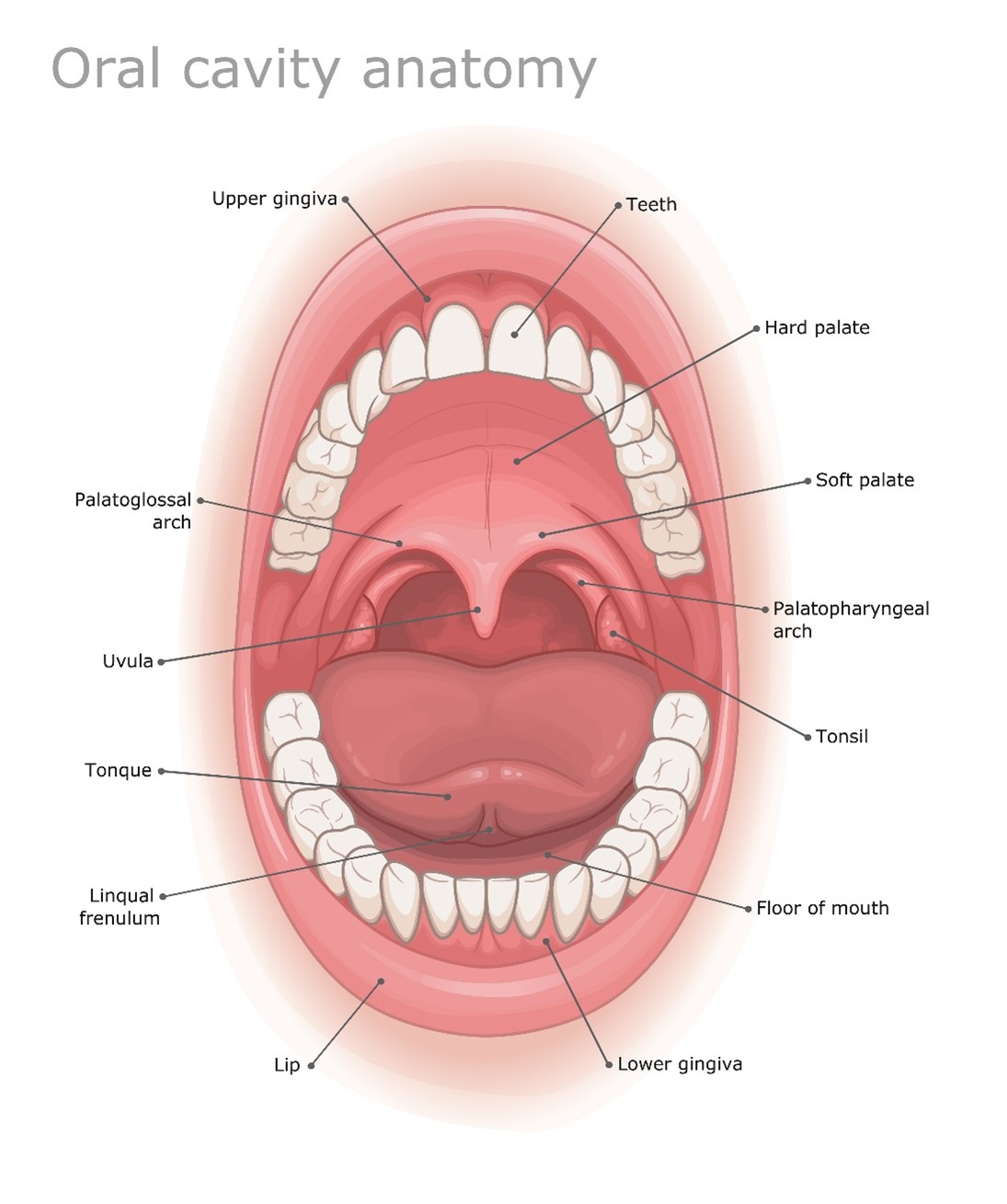
7 Oral Cavity
The oral cavity consists of the lip, floor of mouth, anterior two-thirds of the tongue, buccal mucosa, hard palate, and retromolar trigone; it extends from the lips to the posterior aspect of the hard palate. The circumvallate papillae separate the anterior two-thirds of the tongue, in the oral cavity, from the posterior third of the tongue, which in the oropharynx. The tongue is the most common tissue in the oral cavity to develop malignancy (~25%); the most common spread site is to the cervical lymph nodes. Other routes of lymphatic spread include the buccinator, jugulodigastric, submandibular, and submental nodes. Although lymphatic and hematogenous spread is rare.
Sun exposure carries the most significant risk for the development of carcinomas of the lip. Squamous cell carcinomas of the lip most commonly arise from the lower lip and spread by direct invasion. The upper lip drains into the submandibular and preauricular nodes. The lower lip and anterior mouth drain to the submental nodes. However, the oral cavity has the lowest incidence, except for glottic cancer, of nodal metastasis in the head and neck region. Lymph node involvement increases with large lesions, poorly differentiated tumors, spread to the wet mucosal surfaces, invasion of the dermis, or recurrent disease. Lip cancers are treated like skin cancers, most commonly with surgery. Radiation therapy is used to obtain better cosmesis; surgery may create a significant scar or affect the function and quality of life. Lip lesions are typically treated with superficial x-rays or electrons. The treatment field should include the primary lesion with a 2 cm margin. A teeth shield made of lead and wrapped with a bolus or wax material will absorb backscatter and reduce complications to the teeth and gums. The external beam dose in the treatment of lip cancer is 60-70 Gy at 2 Gy per fraction.
Most oral cavity tumors are candidates for surgical resection as a treatment option. Floor-of-mouth cancers are treated with surgery and radiation therapy. About 30% of these cancers have positive submaxillary and sub digastric nodes. If the lesion is confined to the mouth’s floor, the tongue’s tip is elevated out of the field with a bite plate. However, if the lesion has grown into the tongue, the tongue is flattened with a bite plate and included in the treatment. Typical doses are 50 Gy with a 10-20 Gy boost.
The oral tongue commonly drains to the submandibular and anterior cervical chain nodes. Surgery is preferred for small tumors, including a local excision or hemiglossectomy. Radiation therapy can be used in conjunction with surgery or alone. The treatment decision for oral cavity cancers strongly considers the function of speech and swallowing. The floor of the mouth and oral tongue lesions are usually midline tumors; therefore, bilateral lymph node chains are at risk for disease.
The buccal mucosa is the mucous membrane that lines the inner surface of the cheeks and lips. These tissues are very radiosensitive; therefore, taking adequate care of the area throughout treatment is essential. The initial radiation therapy dose is 55-60 Gy in 6 weeks, followed by a boost of 20 Gy to spare the mandible.
Hard palate carcinomas are rare and originate in the minor salivary glands, primarily adenocarcinomas. They tend to spread to the bone and invade the maxillary antrum. Surgical resection is the most common treatment, with postoperative radiation therapy to 65-70 Gy for high-risk patients. A history of poor-fitting dentures or trauma is common.
The retromolar trigone comprises the tissues of the mandible’s anterior ramus. The triangular subsite extends from behind the mandible’s last molar superiorly to the maxilla’s last molar. Carcinomas in this area are rare. Lymphatic spread occurs in the submaxillary and sub-digastric nodes. Lesions in this area have a high tendency for metastases to the neck; therefore, prophylactic neck treatment is critical. Treatment includes surgical resection and/or radiation therapy to a total dose of 66-74 Gy.
Patient Simulation & Special Considerations: Oral Cavity
The simulation process is consistent with the typical head and neck in treating oral cavity lesions. Please refer to the “Patient Simulation: H&N” section. Additional considerations for oral cavity treatments may indicate using a biteplate or tongue depressor. A bite plate can help keep the mouth open during treatment and make it easier to include or exclude oral mucosa from the treatment field. For example, when irradiating the hard palate, the tongue should be below the tongue depressor to push it inferiorly out of the radiation field. Or when treating the floor of the mouth, the oral tongue can be excluded by moving it above the bite plate. Patients with metal fillings may also benefit from fluoride trays worn during treatment to reduce scatter and irritation to oral tissues.
Treatment Volume Localization: Oral Cavity
The conventional 2D field borders for the floor of mouth and oral tongue lesions include:
-
The general field borders for treatments of the oral tongue. Note: a tongue depressor would move the tongue inferior to reduce dose the the hard palate. The dotted line represents the field extension for node positive disease. Superior: 1.5 cm above the tongue
- Inferior: thyroid notch
- Anterior: in front of the mandible (exclude the lower lip if possible)
- Posterior:
- Node negative: behind the vertebral bodies
- Node positive: behind spinous processes
Treatments today still follow these general borders but are more conformal to targeted tissues, sparing normal tissues and reducing toxicity. Please refer to the “Treatment Volume Location: H&N” section.
Treatment Techniques: Oral Cavity
The dosing may vary depending on the specific site within the oral cavity. Typically, the involved or at-risk lymph nodes are treated to 45-50 Gy, followed by a boost to the gross disease. As a primary treatment for oral cavity cancer, radiation is generally administered daily over 6-7 weeks, to a total dose of 60-70 Gy. Modern treatment techniques are reflected in the “Treatment Techniques: H&N” section.
Media Attributions
- Oral cavity anatomy medical illustration labeled © Анна Богатырева is licensed under a All Rights Reserved license
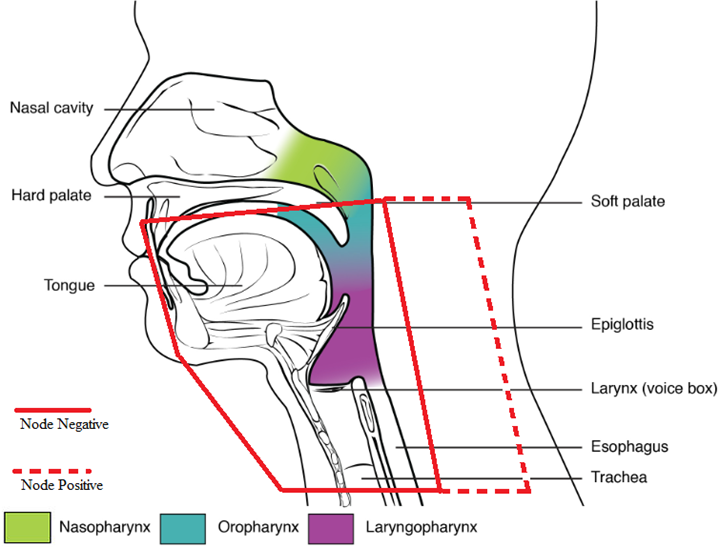
- Divisions of the Pharynx © OpenStax Anatomy & Physiology adapted by Jared Stiles is licensed under a CC BY (Attribution) license
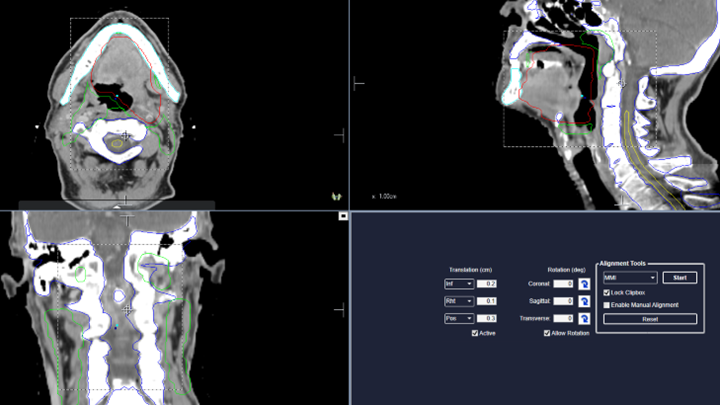
- CBCT image for a malignancy of the oral tongue and tonsil © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
Surgical removal of one half of the tongue

