25 Bladder
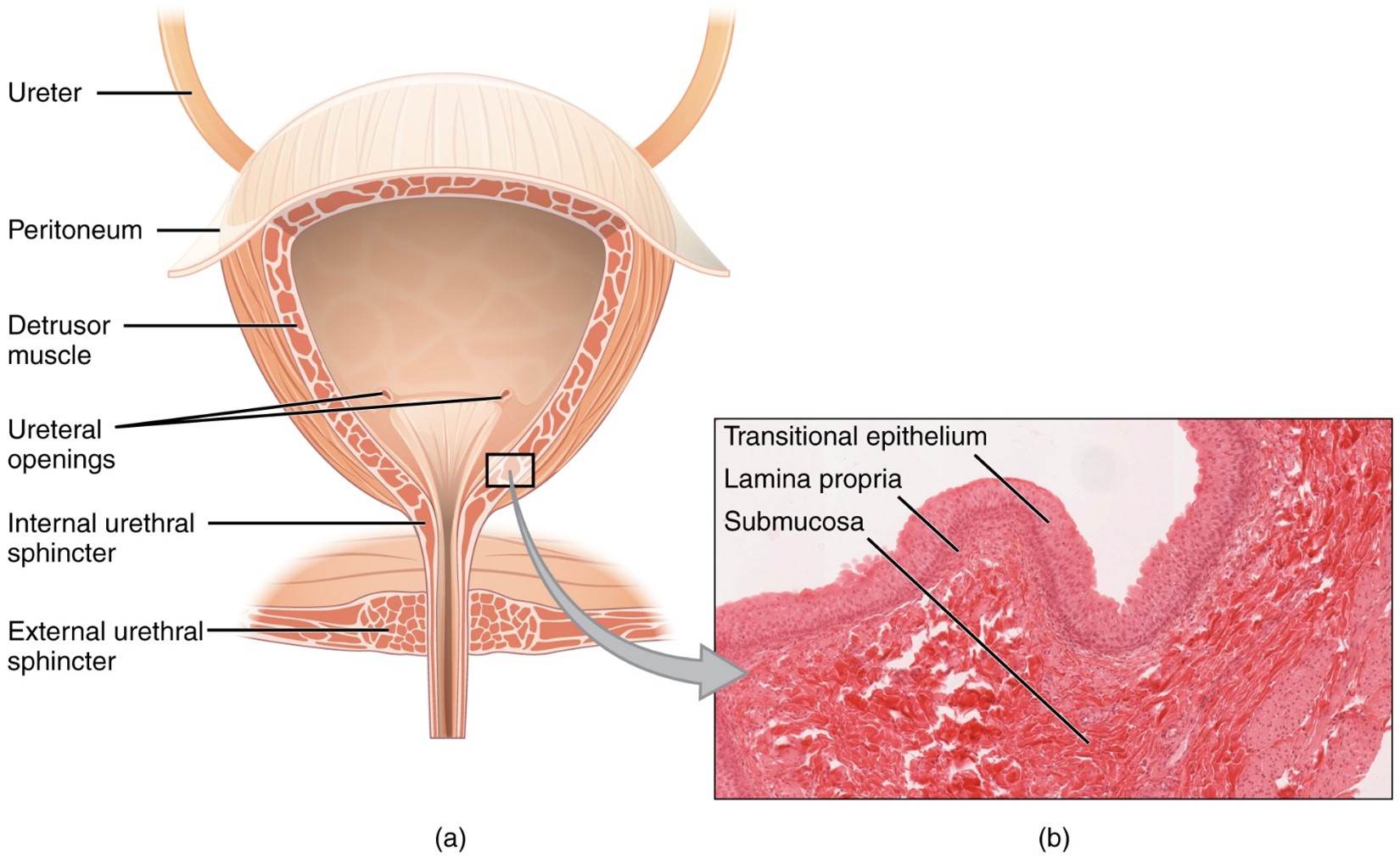
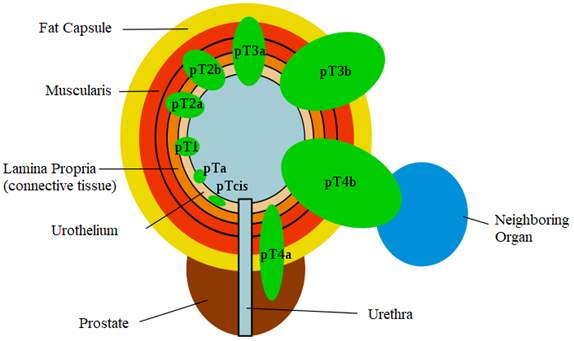
The bladder is located in the true pelvis when empty. The apex of the bladder is located inferiorly and points to the pubic symphysis. Most bladder cancers are found on the trigone in the posterior wall of the bladder (formed from three openings from the two ureters and the urethra). The most common presenting symptom of bladder cancer is gross or microscopic hematuria. Distant metastases include the lung, bone, or liver. Transitional (urothelial) cells are the most common histology, with squamous cell carcinoma, adenocarcinoma, and small cell carcinoma being less common. Important lymphatics to include in the field for bladder cancer are external iliac, common iliac, presacral, and paraaortic nodes.
Patient Simulation & Special Considerations: Bladder
One critical difference for simulation of the bladder is ensuring the patient has an empty bladder when coming in for their simulation and treatment each day. For boost fields, a second simulation and treatment plan may require a full bladder; this helps target the affected tissues and reduces the dose to healthy tissues. The simulation process is otherwise consistent with the typical pelvis setup. Please refer to the “Patient Simulation: Pelvis” section.
Treatment Volume Localization: Bladder
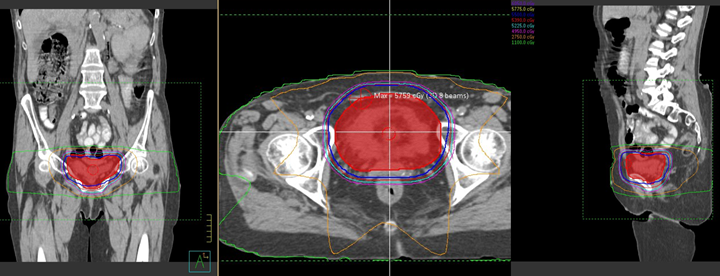
Traditional treatment borders for the bladder are:
- Superior: between S1 and S2
- Inferior: bottom of obturator foramen
- Lateral: one to two centimeters beyond the bony pelvic side walls (Field shaping is usually done around the femurs)
- Anterior: usually extends 1-2 cm beyond the bladder (approximately 1-2 cm anterior to the pubic symphysis)
- Posterior: usually extends 2-3 cm behind the bladder and tumor volume. Dose to surrounding normal tissue and to critical structures, such as the posterior rectal wall, small bowel, and anus should be limited.
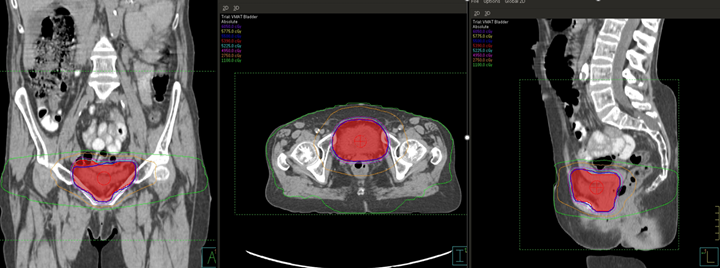
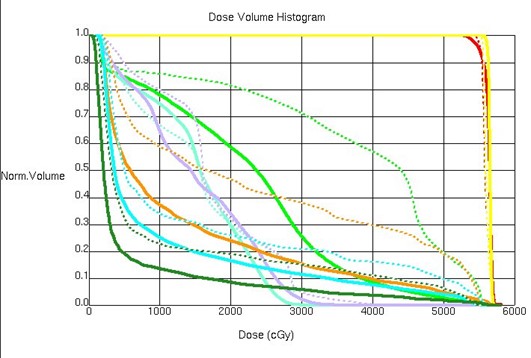
Treatments today still follow these general borders but are more conformal to targeted tissues, sparing normal tissues, and reducing toxicity. Please refer to the “Treatment Volume Localization: Pelvis” section (Anchor 2).
Treatment Techniques: Bladder
The most common treatment for early-stage malignancies of the bladder is by surgical resection via cystoscopy – Transurethral Resection of Bladder Tumor (TURBT). More advanced cancers will benefit from a partial or complete cystectomy and radiation therapy. Doses for the bladder are approximately 55 Gy in 20 fractions over a 4-week period or 64 Gy in 32 fractions over a 6.5-week period. The beam arrangements are consistent with the typical four field arrangement for pelvis cancers. Please refer to the “Treatment Techniques: Pelvis” section.
Media Attributions
- The Bladder © OpenStax College is licensed under a CC BY (Attribution) license
- VMAT plan of the bladder © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- 8-field 3D-CRT plan of the bladder © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Treatment plan comparison © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- TNM Blasenkrebs © Der Reisende adapted by Jared Stiles is licensed under a CC BY (Attribution) license

