2 Whole Brain & Primary Brain Tumors
Patient Simulation: Whole Brain & Primary Brain Tumors
The simulation procedure commonly used for fractionated primary brain tumors includes a CT simulation and/or MR imaging with contrast. The patient’s position and immobilization was provided in the Patient Simulation: CNS section. Scan parameters will extend from vertex to mid-neck (or as specified by physician). Metastatic disease or whole brain patients typically only require a CT sim without contrast. A MRI with contrast for each scan and will provide more insight into tumor vasculature, help differentiate edema from tumor, and enhance soft tissue contrast improving the identification and localization of critical structures. Frequently, CT scans of the brain use intravenous, iodinated, non-ionic, contrast. Therapists should ensure the patient has not received contrast in the last 24 hours, has good kidney function through the verification of lab values (GFR, BUN, Creatinine), and has had nothing to eat or drink (npo) for the last 4 hours. MR scans commonly use gadolinium “gad” contrast.
Treatment Volume Localization: Whole Brain (WBRT)
WBRT will encompass all microscopic disease within the cranial contents. The beam arrangement is a two-field technique using opposed laterals. Treatment field size is approximately 22cm x 17cm.
Treatment borders:
- Posterior, Superior, & Anterior: 1-2cm flash/field falloff (verify with field light)
- Inferior: Superior orbital ridge to 1-2cm below the mastoid tip (verify eye block)

Treatment Techniques: Whole Brain (WBRT)
Radiation therapy for brain metastasis is typically a palliative treatment. Treatment can be given prophylactically for Small Cell Lung Cancers to a dose as low as 20-25 Gy. A slightly lower dose will reduce deficits associated with whole brain radiation therapy and allow for retreatment if metastasis occur later. Standard approach WBRT uses 3000-3750 cGy in 10-15 fx (250 to 300 cGy per fraction). The most common fractionation scheme is 30 Gy in 10 fractions. Other common fraction schemes include:
- 12 Gy: 6 Gy for 2 fractions given on consecutive days
- 20 Gy: 4 Gy/fx for 5 fractions daily
To avoid beam divergence into the opposite eye:
Option 1: Angle each beam posteriorly a few degrees until the beam divergence matches the opposing sides outer canthus. The appropriate angle can be verified in the treatment planning system. Notice, the beams match anteriorly just posterior to the lenses of the eyes. Clinically, this divergence can be matched utilizing two metallic BBs, placed at each eye’s outer canthus, and rotating the gantry using fluoroscopy until they are superimposed.

Option 2: Take advantage of the non-divergence of the central axis of the beam using a half-beam block. Rotate the collimator to match the inferior border (superior orbital ridge and mastoid tip). The isocenter will fall near the EAM. Ensure adequate light field falloff in anterior, superior, and posterior directions.
Emerging Technologies and Treatments: Whole Brain (WBRT):
Hippocampal WBRT is a growing treatment that is focused on sparring the right and left lobes of the hippocampus with the intent of avoiding radiation induced side effects. Like WBRT the entire cranial contents are contoured, Hippocampal WBRT treatment utilizes the Linac’s IMRT functions to limit dose to the hippocampus[1]. Avoidance sectors can help reduce dose to critical structures, like the lenses of the eyes.
Treatment Volume Localization: Primary Brain Tumors
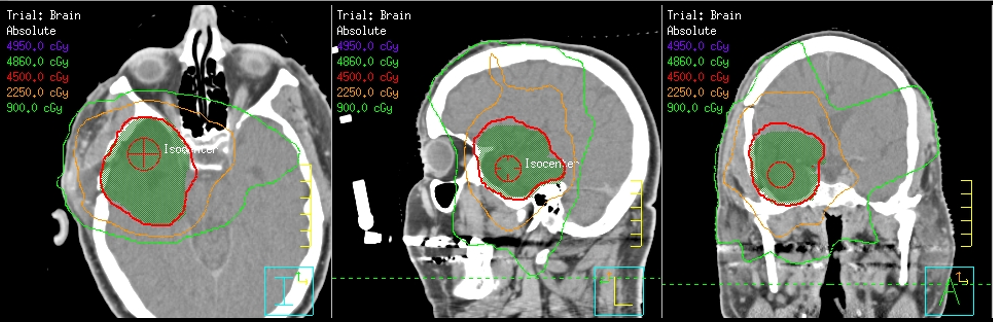
Treatment volumes for fractionated radiotherapy to primary brain tumors can vary by provider and institutional protocols. Historically, contours included the gross tumor volume (GTV) and surrounding edema (determined by pre-operative scans) with a 2-3 cm margin. With advances in technology, treatment margins are much tighter. Today, treatment volumes include the GTV, subclinical disease, and edema, comprising the CTV – clinical tumor volume and a 5mm expansion to the PTV – prescribed tumor volume.
Treatment Techniques: Primary Brain Tumors
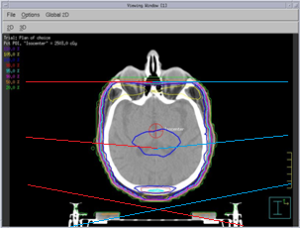
Historically, primary brain tumors were treated with a 2 or 3-field technique; two parallel opposed lateral beams and perhaps a third (anterior, posterior, or vertex) beam. Wedges were common to compensate for the round shape of the head to reduce hot spots and improve dose uniformity. Beam weighting can also achieve help achieve an acceptable dose distribution.
Modern photon treatments incorporate the use of 3D conformal planning using forward-planning. IMRT and VMAT plans using dynamic MLC’s and treatment arcs can be accomplished with inverse-planning. Each type of treatment will have approximately 5 different beams and couch positions. Therapists must take extra caution in the movement of equipment to avoid any potential collisions. Dynamic treatment plans (Rapidarc/VMAT) are more conformal and allow for increased normal tissues sparing and potentially dose escalation.

Low-grade tumors are primarily treated with surgery, but if radiation is needed (due to positive margins or remaining tumor), the dose is to approximately 45-54 Gy at 1.8-2.0 Gy/fx. High-grade tumors are treated to approximately 50 Gy with a 10 Gy boost at 1.8-2.0 Gy/fx. Hypo-fractionation has been found to have similar efficacy; this could shape treatments of the future. Hyper-fractionation and dose escalation have not demonstrated a significant survival benefit.
Emerging Technologies & Treatments: Primary Brain Tumors
- Proton therapy can significantly reduce the dose to normal tissues and is especially advantageous for pediatric patients and CSI treatments.
- MR Linac systems can provide enhanced imaging to detect changes daily and utilize Adaptive Radiation Therapy, generating a new plan and treatment daily based on the image resulting in greater normal tissue sparing and increased target dose.
- Gamma Tiles – Surgically targeted Radiation therapy for patients with operational brain tumors. Inserted by a surgeon at tumor site immediately after removal. Delivers radiation to the targeted area and minimizes side effects.
Media Attributions
- Left and Right lateral whole brain DRRs © University of Iowa Hospitals and Clinics Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Avoiding beam divergence © University of Iowa Hospitals and Clinics Radiation Therapy Program is licensed under a CC BY (Attribution) license
- half-beam block WBRT © Patrick J. Lynch, medical illustrator adapted by Jared Stiles is licensed under a CC BY (Attribution) license
- GBM Isodose lines © University of Iowa Hospitals and Clinics Radiation Therapy Program is licensed under a CC BY (Attribution) license
- GBM beams © University of Iowa Hospitals and Clinics Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Pokhrel, D., Sood, S., McClinton, C., Shen, X., Lominska, C., Saleh, H., Badkul, R., Jiang, H., Mitchell, M., & Wang, F. (2016). Treatment planning strategy for whole-brain radiotherapy with hippocampal sparing and simultaneous integrated boost for multiple brain metastases using intensity-modulated arc therapy. Medical Dosimetry, 41(4), 315–322. https://doi.org/10.1016/j.meddos.2016.08.001. ↵
at present, no evidence of disease; prevents or protects from metastasis
real-time imaging demonstrating motion and/or function
External Auditory Meatus (ear canal)
Breaks in beam output where no monitor units/dose are delivered
the process of applying beams, reviewing isodose line, and modifying to avoid critical structures
the treatment planning process of setting dose constraints on critical structures and the planning system design a treatment plan that meets the plan specifications
fewer fractions at a higher dose
multiple treatments per day

