26 Female Pelvis
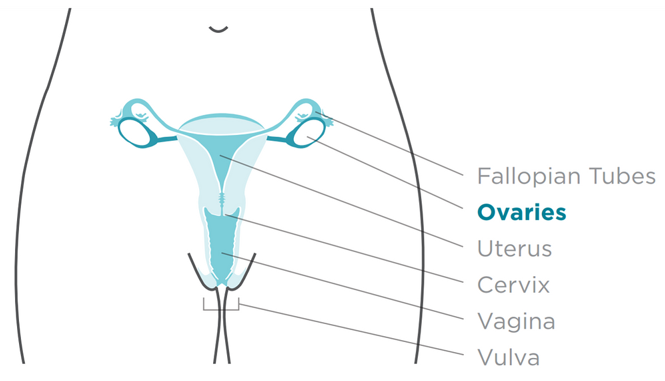
The most to least common gynecological malignancies are endometrial, ovarian, cervical, vulvar, then vaginal. Many risk factors for endometrial cancers are associated with increased estrogen levels over a an extended period; this includes nulliparity, number of menstrual cycles, obesity, hormone therapy, and a history of tamoxifen therapy from a previous breast cancer. The most common histology for endometrial cancers is adenocarcinoma. At the cervix, the tissue type transitions to squamous cell, and the most common pathology for cancers of the cervix, vagina, and vulva are squamous cell carcinomas.
Ovarian cancer is the deadliest gynecological cancer. Risk factors for ovarian cancer include older age, increased exposure to estrogen, history of breast, colon, or endometrial cancers, and genetics (BRCA1 & 2). The most common histology for ovarian cancers is epithelial germ cell. Treatment of these malignancies are covered in the “Whole Abdomen” chapter.
The third most common malignancy in women is cervical cancer. Cervical cancer is correlated with lower socioeconomic status, early sexual activity, and HPV infection. Signs and symptoms commonly associated with gynecological lesions include bleeding, pelvic pain, mass, etc. The staging system used for gynecological malignancies is the FIGO (International Federation of Gynecology and Obstetrics) staging system.
The most common patterns of spread for cancers of the female pelvis include direct extension, lymphatic spread, hematogenous spread, and distant spread. Intraperitoneal seeding can also deposit tumors along the recesses of the peritoneum; these metastases can manifest as soft tissue nodules or plaque masses. Lymphatic channels serve as routes of spread for pelvic disease as spread can occur along the ligaments and the mesentery. Common sites of distant metastatic disease include the lungs, the pelvic and para-aortic lymph nodes, and the peritoneum. Local recurrence is often a common concern.
|
OAR (Organ at Risk)
|
TD 5/5 (Whole Organ)
|
Outcome Associated
|
|
Rectum
|
60 Gy
|
Proctitis, necrosis, fistula |
|
Colon
|
45 Gy
|
Obstruction, ulceration, perforation/fistula |
|
Bladder
|
65 Gy
|
Cystitis, ulcer, perforation/fistula |
|
Femoral Heads
|
52 Gy
|
Necrosis |
|
Small Bowel
|
40 Gy
|
Obstruction, ulceration, perforation/fistula |
|
Ovaries
|
2 Gy
|
Sterility, early menopause |
| Vulva / Skin |
55 Gy
|
Fibrosis
|
|
Uterus, Cervix, and Vagina can tolerate very high treatment doses (>140 Gy); Fibrosis, ulceration, and fistula may develop
|
||
Overview: Endometrium & Cervix
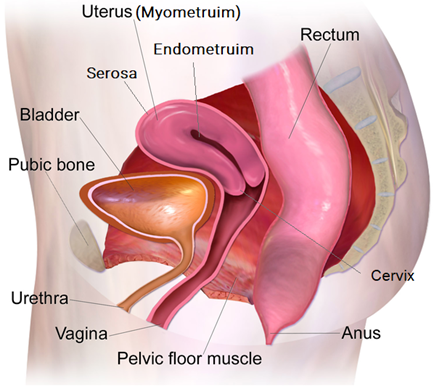
The most common gynecologic malignancies treated with radiation therapy are cervical and endometrial cancers. The uterus is located in the true pelvis, posterior to the bladder and anterior to the rectum. The three portions of the uterus are the fundus, corpus, and cervix. The body of the uterus has three layers: endometrium, myometrium, and serosa.
Carcinoma of the endometrium is the most common malignant lesion that arises from the female genital tract. The most common histology for endometrial cancers is adenocarcinoma. The most common routes of spread are by direct extension into the cervix, vagina, bladder, and rectum, lymphatics, and transperitoneal spread. The lymphatics that are commonly involved are the external iliac, internal iliac, common iliac, and periaortic lymph nodes. Endometrial cancer uses the FIGO staging system to describe the extent of the disease. The following link provides a breakdown of the stages: Endometrial Cancer Stages.
Cervical cancer is the third most common cancer in women worldwide. However, invasive cervix carcinoma has decreased significantly with the advent of screening; current recommendations of the American Cancer Society include a pap smear starting at 25 years old. Chronic HPV (human papillomavirus) is a significant risk factor for cervical cancer; most cases are found in developing countries where preventative vaccinations are unavailable. HPV+ patients have an improved prognosis.
Squamous cell carcinoma is the most common pathologic type of cervical cancer. A rich lymphatic system encompasses the cervix and uterus. The three most frequently involved nodal groups are the obturator and internal and external iliac nodes. Cervical cancer uses the FIGO staging system to describe the extent of the disease. The following link provides a breakdown of the stages: Cervical Cancer Stages | How to Stage Cervical Cancer.
Patient Simulation & Special Considerations: Endometrium & Cervix
For advanced cervical cancers, the para-aortic lymph nodes may require treatment; if so, position the patient with their arms above their head and add straightening marks to the superior abdomen. Using a knee bolster can help the patient flatten their spine and improve comfort and reproducibility. Additionally, a radiopaque marker may be inserted onto the vaginal apex to help identify the area by CT scan. The simulation process is otherwise consistent with the typical pelvis in treating endometrial and cervical cancers. Please refer to the “Patient Simulation: Pelvis” section.
During simulation for brachytherapy, the patient will be in a supine position with the vaginal applicators in place. Image-guidance is provided with AP kV images, CT, and/or MRI to confirm the applicator is in the correct position or if any changes need to be made. These images should contain the entire brachytherapy applicators(s) and critical structures including the bladder and rectum.
Treatment Volume Localization: Endometrium & Cervix
Traditional treatment borders for the endometrium and cervix 4-field “box” are:
Endometrial cancer treatment fields:
- Superior: L5-S1 interspace to include the common iliac nodes
- Inferior: bottom of the obturator to include the common iliac nodes
- Lateral: a minimum of 1 cm lateral to the pelvic brim to encompass the external and internal iliac nodes.
- Anterior: encompass the symphysis pubis
- Posterior: split the sacrum
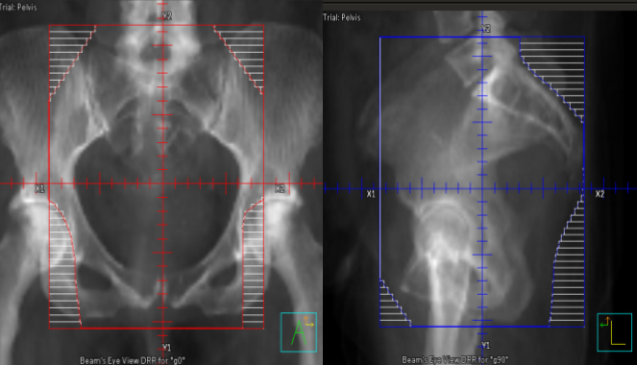
Cervical cancer treatment fields:
- Superior: L4-L5 interspace
- Inferior: the bottom of the obturator foramen
- Lateral: 1-2 cm lateral to the pelvic inlet
- Anterior: encompassing the pubic symphysis
- Posterior: split the sacrum
*If there is disease superior or inferiorly, the borders are adjusted to include all disease with a 1-2 cm margin.
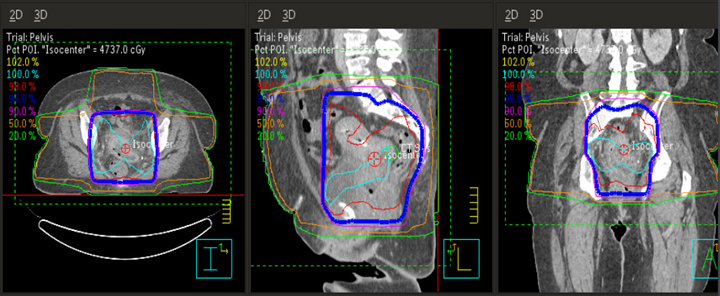
Treatments today still follow these general borders but are more conformal to targeted tissues, sparing normal tissues, and reducing toxicity. Please refer to the “Treatment Volume Localization: Pelvis” section.
Treatment Techniques: Endometrium & Cervix
The most common treatment for endometrial and cervical cancer is surgery. Some surgical interventions include a wedge resection and a total or partial hysterectomy. When radiation therapy is used as an adjuvant form of treatment, the tumor and regional lymphatics are typically treated to 45-50 Gy at 1.8-2.0 Gy per day, and the primary tumor can be boosted with intracavitary brachytherapy to doses of 80-85 Gy. Most patients also receive concurrent chemotherapy as a radiosensitizer (the patient needs chemo before RT), which helps produce more favorable outcomes. Late side effects of pelvic irradiation include ulceration or thickening, potentially evolving into a bowel obstruction or fistula.
The treatment techniques are consistent with the standard pelvis protocol in treating the endometrium and cervix. Modern treatment techniques are reflected in the “Treatment Techniques: Pelvis” section.
Overview: Vagina
The vagina is a muscular tube about 7.5 inches long that forms a passageway from the vulva to the uterus, and it is located posterior to the bladder and anterior to the rectum. Vaginal cancer is very rare and can be associated with smoking, HPV, and exposure to the drug diethylstilbestrol (DES) in utero. The most common histopathology is squamous cell carcinoma, and the inguinal lymph nodes are the lymph nodes most frequently involved. Some signs and symptoms of vaginal cancer include vaginal bleeding, discharge, mass, pain during intercourse, and painful urination. Vaginal cancer spreads via direct extension into nearby tissues, and squamous cell carcinomas tend to metastasize to the lungs, the liver, and the supraclavicular lymph nodes. Vaginal cancers use the FIGO staging system: Vaginal Cancer Stages.
Patient Simulation & Special Considerations: Vagina
Patients are positioned supine with their legs abducted slightly to reduce perineal skin reactions from treatment. Legs are immobilized with custom-made vaclok or alpha cradle, using a radiopaque marker placed on the inferior extent of the vaginal tumor to help identify the GTV margin dosimetrically. Lateral positioning marks reduce leg rotation and improve reproducibility. Intravenous contrast administration enhances the visibility of the blood vessels on the CT images. The simulation process is otherwise consistent with the typical pelvis. Please refer to the “Patient Simulation: Pelvis” section.
For brachytherapy procedures, patients are simulated with the applicator, a “cylinder” inserted, and an external fixation device to prevent the applicator from moving. A Foley catheter is inserted into the bladder at the beginning of the procedure. During the simulation and treatment, the doctor will fill the bladder to move surrounding structures away from the source and reduce the dose to normal tissues. During the planning phase, the bladder can drain empty.
Treatment Volume Localization: Vagina
For external beam radiation therapy, the PTV, bowel, rectum, bladder, femoral heads, and bone marrow are organs-at-risk. For three-dimensional conformal radiation therapy, the field-in-field technique is utilized to decrease the occurrence of hot-spots and to reduce the bowel dose. For brachytherapy, the CTV, the sigmoid, rectum, and bladder are all considered organs-at-risk. When creating a brachytherapy plan, the treatment planning system provides a manual optimization plan to reduce dose to the critical structures. Treatments are either intracavity and using an applicator called a cylinder, or interstitial using needles and catheters.
Treatment Techniques: Vagina
Carcinoma of the vagina is typically treated using external beam radiation therapy to the entire pelvis, which includes the associated lymph nodes, to a dose of 45-50.4 Gy in 25-28 fractions at 1.8 Gy per fraction. If a boost is necessary and delivered via an external beam, the dose is an additional 15-20 Gy in 8-11 fractions.
Brachytherapy, if used as the primary form of treatment, uses either a low-dose-rate to 60 Gy or a high-dose-rate to 33 Gy in 6 fractions over 10-19 days. If used as a boost, low-dose-rate (LDR) brachytherapy is given in doses of 15-25 Gy, depending on the location of the applicator. High-dose rate (HDR) brachytherapy is given in doses of 11 Gy in 2 fractions or 16.5 Gy in 3 fractions depending on technique, either intracavitary or interstitial. Interstitial applicators are used when intracavitary applicators do not fit correctly, the tumor is too large, or the tumor is too superficial or deep. Interstitial treatments have improved coverage of the diseased area and decreased the dose to the organs at risk.
Palliative treatment is also an option for affected patients. The doses and fractionation schemes for vaginal disease are:
Palliative External Beam Radiation Therapy (EBRT):
- 20 Gy in 5 fractions
- 30 Gy in 10 fractions
- 8-10 Gy in 1 fraction for hemostasis
Brachytherapy (interstitial or intracavitary):
- LDR: 20-30 Gy
- HDR: 18-24 Gy in 3-4 fractions
Overview: Vulva
The vulva is the outer portion of female genitalia, including the labia, the clitoris, the vaginal opening, and the opening to the urethra. Vulvar cancer accounts for 4% of all gynecological cancers, it most commonly affects women over the age of 70, and 90% of all vulvar cancers are squamous cell carcinoma. Carcinoma of the vulva are primarily treated by surgical resection, with or without adjuvant radiation therapy. Early-stage disease is treated with wide, local excision. Postoperative external beam radiation therapy is recommended for residual or recurrent disease.
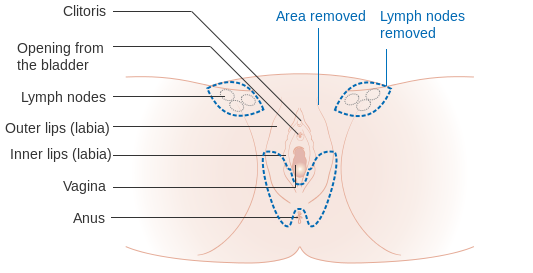
Vulvar cancer spreads via lymphatics to the superficial inguinal lymph nodes, deep femoral lymph nodes, and pelvic lymph nodes. Spread can also occur by direct extension to neighboring structures like the urethra, anus, or vagina. Hematogenous spread is rare. Vulvar cancer is associated with smoking and HPV, and some signs and symptoms include red, white, or pink bumps, itching, bleeding, and discharge. Vulvar cancer uses the FIGO staging system: Vulvar Cancer Stages.
Patient Simulation & Special Considerations: Vulva
Patients are typically positioned supine with legs akimbo or “frog leg” to reduce skin folds and scatter dose. Bolus placement is also easier. Bolus will bring the dose more superficial to the surface tissues and eliminate cold spots in the treatment area. During simulation, stirrups and a custom-made vaclok can immobilize the patient’s legs and increase reproducibility in subsequent treatments. If treating with an electron, a feet-first position on the table may be necessary. For additional information regarding the simulation of the pelvis, please refer to the “Patient Simulation: Pelvis” section.


Treatment Volume Localization: Vulva
Beam arrangements for advanced cancers of the vulva are AP/PA. Treatment borders for a 3D conformal plan are:
- Superior: L5-S1 interspace to include the common iliac lymph nodes
- Inferior: Bottom of the obturator foramen or perineum
- Lateral Anterior: to include inguinal lymph nodes
- Lateral Posterior: narrow to protect femoral necks
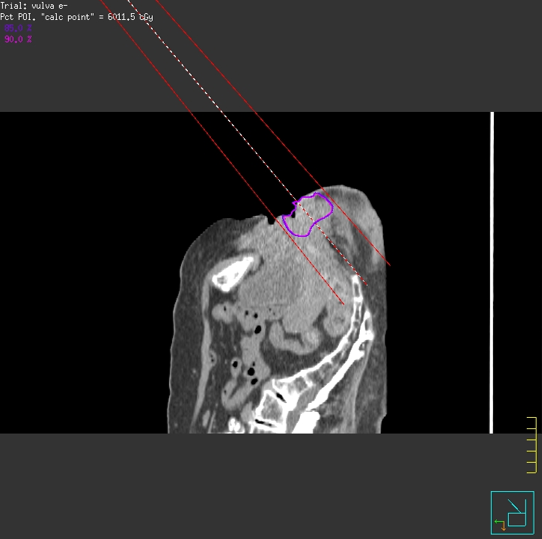
Treatment Techniques: Vulva
Vulvar radiation therapy commonly utilizes 3D conformal or IMRT/VMAT 6 MV technique to treat the superficial tissues, lymph nodes, and pelvic disease. Both help shape the radiation beams and limit the dose to healthy tissues like the bowel, rectum, and bladder. Doses beyond 40 Gy often require treatment breaks due to moist desquamation. Doses and fractionation schemes for vulvar disease are as follows:
- When the resection margins are insufficient, the postoperative dose is 45-50 Gy 6 MV with an electron boost of 10-20 Gy.
- For electron treatments, the dose is 50-60 Gy, which includes the boost.
Media Attributions
- Site of Ovarian Cancer © Centers for Disease Control and Prevention is licensed under a Public Domain license
- Pelvic Muscles (Female Side) © BruceBlaus adapted by Jared Stiles is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
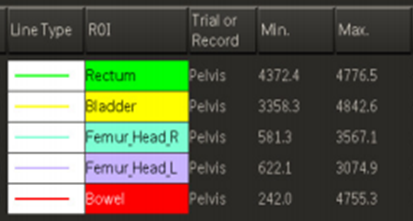
- Pelvis Images © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- 4-field pelvis isodose plan for cervical cancer with equal weighting. © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
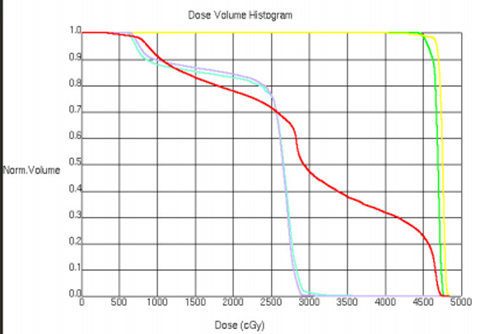
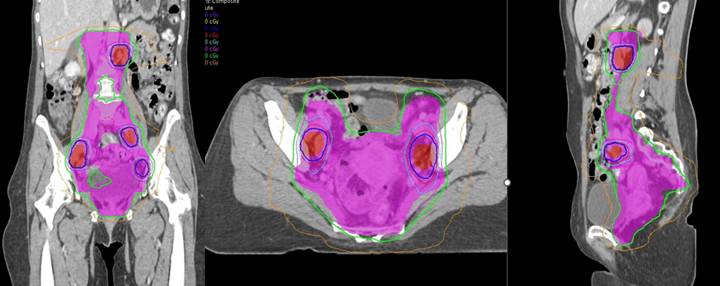
- DVH for cervical cancer to include the para-aortic lymph nodes. © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- DVH structures for cervical cancer to include the para-aortic lymph nodes. © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- VMAT treatment for cervical cancer to include the para-aortic lymph nodes. © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Diagram showing a simple or partial vulvectomy when the cancer is affecting the bottom part of the vulva and perineal area CRUK 079 © Cancer Research UK is licensed under a CC BY-SA (Attribution ShareAlike) license
- Legs Akimbo © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Legs Akimbo Anterior © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Electron treatment of the vulva © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
Describes a woman who hasn't given birth to a child
A hormone therapy drug used to treat hormone receptor-positive breast cancer
A global organization combining professional societies of obstetricians and gynecologists

