18 Overview: Abdomen
- Describe the anatomy, structures, and landmarks of the abdomen
- Describe malignancies of the abdomen
- Describe the simulation process of the abdomen
- Identify commonly used positioning & immobilization devices used for abdominal treatments
- Define scan parameters and reference isocenter location for abdominal simulations
- Discuss special considerations in abdominal patient positioning
- Define the “traditional” treatment borders and how they relate to tumor spread
- Describe tumor volumes and margins for abdominal tumors
- Discuss the various treatment procedures of abdominal malignancies
- Perform tasks associated with the simulation and treatment of abdominal malignancies
Key Terms
- Anastomosis
- Adapt to Position
- Adapt to Shape
- Embolization
- Enteritis
- Intraperitoneal
- Magnetic Resonance-guided Radiation Therapy (MRgRT)
- MIBG Radiotherapy
- Nephrectomy
- Neuroblastoma
- NPO
- Palliative Whole Abdomen Irradiation
- Retroperitoneal
- TIGER-PaC
- Whipple Procedure
- Whole Abdomen Irradiation (WAI)
- Wilms Tumor
Overview: Abdomen
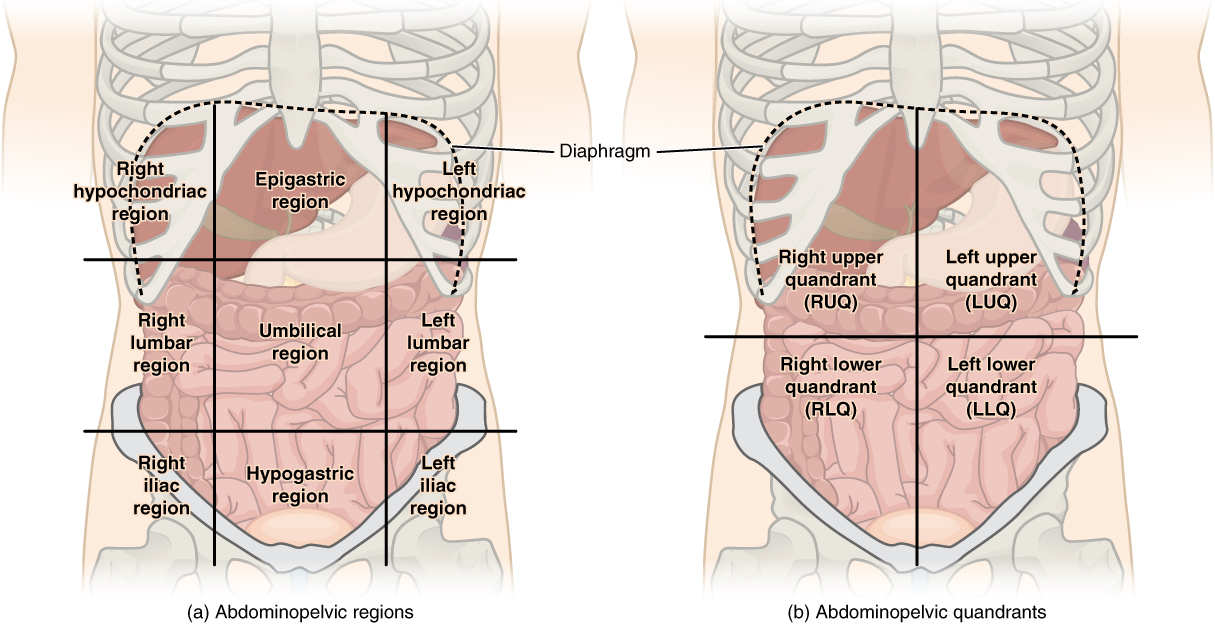
The abdomen is commonly described anatomically in four quadrants; the Right Upper Quadrant, Left Upper Quadrant, Right Lower Quadrant, and Left Lower Quadrant. The major components of the abdomen include the pancreas, kidneys, liver, gallbladder, stomach, intestines, and colon. These tissues have a rich lymphatic drainage that converges at the cisterna chyli at the second lumbar vertebra before draining to the thoracic duct.
Learn more abdominal anatomy by visiting this website.
Patients undergoing abdomen cancer treatment are first changed into a gown. Ensure the patient’s waste bands, zippers, or buttons, are out of the field of view and not moving the patients tissues. Begin by positioning the patient supine with arms above their head in an indexed wing board or arm board. A vaclok or a knee bolster under the legs will improve comfort and help flatten the back to improve reproducibility. While these are the most commonly utilized immobilization devices, other options exists and are depending upon the patient’s ability, equipment availability, and doctor preference.
The patient’s upper half is uncovered, and their lower half should expose midthigh; protect the patient’s modesty as much as possible. Three reference marks are placed at a stable position on the patient’s skin; laterally on each side and anteriorly. Straightening marks are also placed superior and inferior to the anterior isocenter for straightening. Abdomen marks can be unstable depending on a patient’s body size and habitus. Patients with a larger body habitus, especially in the abdominal area, will likely have a less reliable and reproducible anterior mark. The CT scan parameters generally range from above the diaphragm to below the iliac crest depending upon the treatment site.

It is common for the doctor to request IV and oral contrast when simulating a patient for abdominal treatment. Oral contrast should be given before the simulation, but IV contrast should be given after the tomogram image is completed. Contrast enhances blood, vessels, intestines, and specific organs to assist the doctor when designing the treatment plan.
Special Simulation Considerations: Abdomen
One of the most common considerations in treatments of the abdomen is tumor motion due to respiratory motion. Various methods exists to reduce tumor motion during treatment. These techniques include abdominal compression, active breathing control, deep-inspiration breath hold, and respiratory gating with tumor tracking. Motion management is often patient-specific, and the chosen technique is often the one that is best suited for the patient. These are techniques are further described in the Special Simulation Considerations: Thorax section.
This video describes the ANZAI Respiratory Gating System. It simulates the technology for a breast patient, however, the same technique is used for abdominal treatments following the same process. This link describes the ANZAI Respiratory Gating System; its general purpose, involved equipment, and clinical workflow.
In addition to respiratory motion, peristalsis and eating before treatment can cause motion or a shift in anatomical position of some anatomy. Some patients are instructed not to eat two to four hours before treatment or NPO, meaning nothing by mouth. Not eating before treatment can also help reduce nausea induced by the radiation. Always be sure to communicate these instructions to the patient before their simulation as well as each treatment.
 Patients who cannot bring their arms above their head can be positioned with their arms high on their chest with hands clasped if treating the lower abdomen. If the treatment area is in the upper abdomen, the patient can clasp the opposite arms elbows wresting their forearms on their forehead. A headrest and vaclok under the patients head can help support the arms and improve reproducibility.
Patients who cannot bring their arms above their head can be positioned with their arms high on their chest with hands clasped if treating the lower abdomen. If the treatment area is in the upper abdomen, the patient can clasp the opposite arms elbows wresting their forearms on their forehead. A headrest and vaclok under the patients head can help support the arms and improve reproducibility.
Treatment Volume Localization: Abdomen
Cancers of the abdomen have varying margins depending on the treatment intent – palliative or curative. Margins also depend on the treatment technique and surrounding anatomy. Treatment design is based on the location of the primary tumor, surrounding critical structures, and the lymphatic drainage of the primary site. Tumor motion is considered during treatment planning and will be used if determined beneficial. Due to the contents of the abdomen, conformal treatments are preferred to limit side effects and spare healthy tissue and unaffected organs. For this reason, VMAT is the treatment of choice for curative treatments of abdominal cancers.
|
Organs at Risk (OARs)
|
TD 5/5 (Whole Organ)
|
Outcome Associated
|
|
Kidney
|
23 Gy – One Kidney
18 Gy – Mean dose to both Kidneys
|
Renal Insufficiency
|
|
Liver
|
30 Gy
|
Hepatitis
|
|
Lung
|
18 Gy
|
Pneumonitis
|
|
Heart
|
40 Gy
|
Pericarditis
|
|
Stomach
|
55 Gy
|
Perforation/Stricture
|
|
Rectum
|
55 Gy
|
Diarrhea
|
|
Bladder
|
65 Gy
|
Cystitis/Stricture
|
|
Femoral Heads
|
52 Gy
|
Osteonecrosis
|
|
Small Bowel
|
40 Gy
|
Obstruction/Perforation
|
|
Large Bowel (Colon)
|
50 Gy
|
Obstruction/Perforation
|
|
Spinal Cord
|
45 or 47 Gy
|
Transverse Myelitis
|
|
Ovaries
|
2-3 Gy
|
Sterilization
|
Treatment Techniques: Abdomen
Due to the critical structures in the abdomen, nausea is a common side effect of radiation. The dose rate can affect the intensity of the nausea. Patients typically begin with a standard dose rate, with their symptoms monitored throughout treatment. If nausea occurs, anti-nausea medications an hour or two before treatment can reduce these affects. If nausea persists, the radiation oncologists can prescribe to lower the dose rate. Typically a dose rate lower than 300 MU/min ran reduce the patient’s nausea. However, this does increase the time it takes to deliver the patient’s treatment.
Most treatments today use daily imaging before treatment – Image-Guided Radiation Therapy (IGRT). Depending on tumor location, the structures to align daily imaging to may vary. The spine is always a reliable starting reference point. It is vital to double-check your longitudinal alignment with at least one other reference point, such as the carina, lung/diaphragm, 12th rib, kidneys, liver edge, or iliac crest. From here, patient alignment should focus on the PTV and the surrounding structures.
- Palliation (AP/PA): This beam arrangement is commonly reserved for pain relief and symptom reduction; doses are 20-30 Gy in 5-10 fractions.
- 3D Conformal: Treatments utilizes multiple beam angles and fields to create a conformal dose distribution.
- VMAT: Curative abdominal treatments are often delivered via the VMAT technique due to the abundance of critical structures. VMAT can deliver radiation quickly from various angles while using MLCs to shape the beam. A significant benefit of this technique is its ability to spare normal tissue and keep side effects to a minimum, which is especially important in the abdominal region.
- SBRT: Lesions < 5 cm are generally eligible for treatment using SBRT. The energy is typically 7-10 MV using a flattening-free-filter (10 MV) beam. Most lesions of the abdomen treated with this technique are located in the liver. They are further described in the SBRT unit.
Surface monitoring systems assist during patient setup and monitor the patient’s position throughout treatment. Surface monitoring systems can track surface motion and position with <1 mm accuracy. These systems use a 3D model of the patient acquired during their CT simulation. A red light projects onto the patient’s skin surface and records their surface position. The systems monitor the pitch, yaw, and roll of the patient. Pitch is the back elevation, yaw is the hip adjustment, and roll is the patient’s rotation. During treatment setup, surface monitoring systems assist in reproducing the patient’s position. After daily imaging and completing table adjustments, a new image capture is taken for treatment. The image is used as a baseline to monitor patient movement during treatment – this is required daily. Some clinics utilize surface monitoring systems that automatically interrupt the radiation beam if the patient moves out of tolerance.
Motion monitoring systems like respiratory gating (previously described) and live imaging continue to make advances.
Proton Therapy: Motion improvement techniques for pencil beam scanned proton therapy should be evaluated and selected based on organ motion. Organ movements to be assessed for proton therapy include those of the target and all organs in the potential proton beam path. For example, treating the lower esophagus using posterior fields where the diaphragm moves severely impacts the delivered beam range relative to the treatment target.
Magnetic Resonance-guided Radiation Therapy (MRgRT): Due to abdominal organs’ movability and placement, a popular emerging treatment option is to treat these patients with MRgRT. The radiation delivery via a magnetic resonance linear accelerator (MR-Linac) uses magnetic resonance imaging with radiation to treat cancer patients. A significant benefit of this treatment technique is the ability to provide motion management and real-time imaging during treatment to ensure the target remains in the treatment field and sparing healthy tissue. It also allows the treatment to “Adapt to Shape” or “Adapt to Position” before each fraction. This is ideal for these cancers because the stomach may be in a slightly different position each day.
Media Attributions
- Abdominal_Quadrant_Regions © OpenStax via Wikimedia Commons is licensed under a CC BY (Attribution) license
- wingboard © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- arms on forehead anterior © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
the surgical connection of two channel-like structures
One of the two treatment plan workflows for MR-Linac treatments that moves the contours to the new target position for that day
The second treatment plan workflow for MR-Linac treatments that adapts the contours and plan to the new patient anatomy
A minimally invasive procedure that blocks a blood vessel
Inflammation of the small intestine
Intraperitoneal contents are within the thin, transparent peritoneum of the abdominal cavity containing the abdominal organs
A type of radiation treatment that uses MRI with a linear accelerator to treat cancer
A type of internal radiation therapy that uses iodine-131 combined with MIBG (Meta-Iodo-Benzyl-Guanidine) to treat neuroblastoma
surgical removal of a kidney
A cancer found in infants and young children because it develops in immature nerve cells throughout the body
nothing by mouth
Radiation treatment to the whole abdomen including each diaphragm and the pubic bone used to relieve pain, treat locally advanced disease and historically to treat ovarian cancer
located behind the peritoneum
A phase III clinical trial targeted treatment for pancreatic cancer
The surgical procedure used to treat pancreatic cancer
Radiation treatment to the whole abdomen including each diaphragm and the pubic bone used to treat locally advanced disease and historically to treat ovarian cancer
A childhood cancer found in the kidneys

