5 Overview: Head & Neck
Learning Objectives
- Describe the anatomy, structures, and landmarks of the head & neck
- Describe malignancies of the head & neck
- Describe the simulation process
- Identify commonly used positioning and immobilization devices used for head & neck treatments
- Discuss special considerations in head & neck patient positioning
- Define scan parameters and reference isocenter location for head & neck simulations
- Define the treatment borders and how they relate to tumor spread
- Describe tumor volumes and margins of head & neck tumors
- Discuss the various treatment procedures of head & neck malignancies
- Perform tasks associated with the simulation and treatment of head & neck malignancies
Key Terms
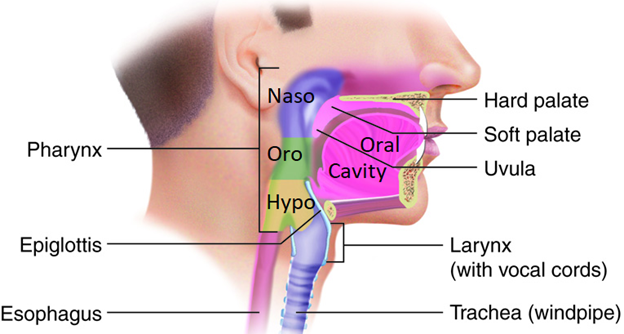
Cancer treatment of the head and neck (H&N) is challenging because of the number of critical structures and proximity of different tissues with varying radiosensitivity. Tumors in the head and neck region are additionally challenging because this area is difficult to access with surgery. Thus, radiation therapy is indicated in most head and neck cancers. The head and neck are comprised of many anatomical sites, including the paranasal sinuses, nasopharynx, oral cavity, oropharynx, larynx, hypopharynx, and parotid glands. The prognosis generally decreases as the affected area progresses backward from the lips to the hypopharynx, excluding the larynx. The lungs are the most common site of distant metastasis. The most significant incidence of head and neck cancers is in the oral cavity and oropharynx. Incidence rates for the oral cavity and oropharynx are more than twice as high in men than in women.
Most head and neck cancers are squamous cell carcinoma, which arises from the epithelial cells of the upper aerodigestive tract. Adenocarcinomas comprise 7% of head and neck cancers, most of which are found in the salivary glands. There are numerous other less common histological subtypes within the head and neck. These cancers grow fast, most with a doubling-time of three to five days; therefore, it’s vital to avoid significant breaks in treatment.
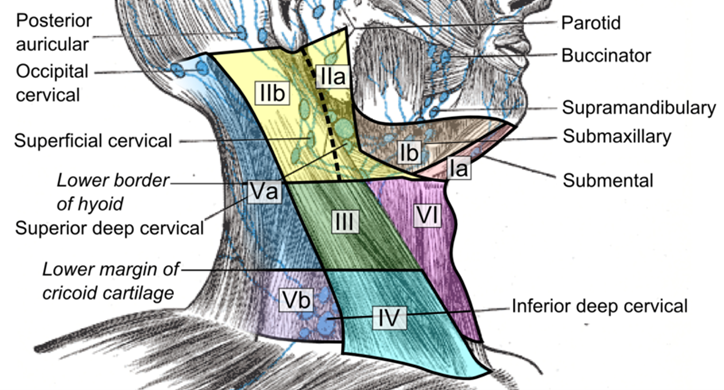
Nearly one-third of the body’s lymph nodes are in the head and neck. Drainage usually occurs ipsilaterally, but some structures, such as the tonsils, the base of tongue, and the posterior pharyngeal wall, have bilateral drainage. True vocal cord (TVC), paranasal sinuses, and the middle ear have little to no lymphatic drainage. Treatment of the lymph nodes in primary head and neck cancers depends on many factors, including cell type and differentiation, size of the primary tumor, lymphatic vascular space invasion of cancer, the extent of primary disease, the site of primary disease, and the clinical or present nodal status of the patient. The jugulodigastric lymph node or sub-digastric node is located below the mastoid tip near the angle of the mandible; it receives almost all the lymphatic drainage from the head and neck area. Therefore, this node is commonly involved in the treatment fields. Another important lymph node is the Node of Rouviere or the retropharyngeal lymph nodes. These nodes cannot be surgically removed, which leads to a high risk of distant metastasis; therefore, they should be included in the treatment fields. Learn more about lymph node levels of the neck.
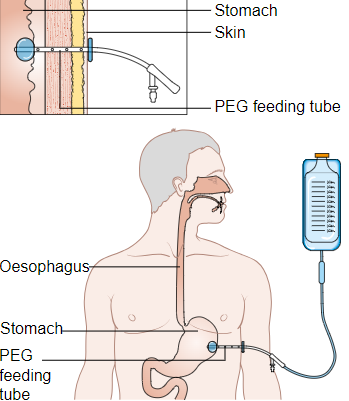
Many head and neck patients already have nutritional deficiencies. These deficiencies can be amplified due to side effects related to RT treatment. It is common for patients to have a percutaneous endoscopic gastrostomy (PEG) tube placement before or during treatment due to side effects that make eating painful and difficult. Because of these side effects, it is common for patients to lose weight, possibly requiring a new treatment simulation, mask, and treatment plan. General risk factors for head and neck cancer include tobacco and alcohol use, ultraviolet light exposure, viral infections, and environmental exposures. Tobacco and alcohol are two of the most significant risk factors. When used jointly, tobacco and alcohol have a synergistic effect, amplifying the impact each will have on developing diseases. Epstein-Barr virus (EBV), herpes simplex virus 1 (HSV-1), and human papillomavirus (HPV) have also been linked to head and neck carcinogenesis and have an improved prognosis using targeted therapies.
Clinical presentation is dependent on anatomical location. Symptoms by site may include:
Nasopharynx:
- Neck mass is the number one presenting symptom
- Epistaxis or bleeding form the nose
- Nasal obstruction
- Unilateral decreased hearing and otitis media due to eustachian tube compression
- Pain
- Headache due to clival or skull bone invasion
- Hearing changes
- Trismus if the pterygoid or masticator space is involved
- Cranial nerve deficits when there is skull base and cavernous sinus invasion
- Leukoplakia or erythroplakia
- Non-healing sores or ulcers
- Halitosis
- Pain
- Dysphagia
- Neck mass is the number one presenting symptom
- Sore throat
- Dysphagia and/or odynophagia
- Otalgia or ear pain when the cranial nerve IX (glossopharyngeal nerve) is involved
- Hot Potato voice and hoarseness are associated with later stage, bulky base of tongue, or larynx involvement. It is noted this is not associated with HPV positive diseases
Larynx/Hypopharynx:
- Glottic cancers present with hoarseness as number symptom
- Supraglottic/hypopharyngeal cancers typically present with sore throat
- Dysphagia/odynophagia
- Cough
- Hemoptysis
- Neck mass
| Grade | Features of Grade |
| Grade I | Well differentiated |
| Grade II | Moderately differentiated |
| Grade III | Poorly Differentiated |
Patient Simulation: H&N
The simulation process is an essential part of a patient’s treatment plan. The simulation is performed after the patient has met with the doctor and consented to treatment. The physician completes an image request for simulation specifying treatment setup and intended delivery. The request should include the patient’s specific treatment site, contrast orders (if indicated), type of immobilization devices, scan parameters, and any special instructions regarding setup. Standards and similarities exist across the profession, but differences could occur due to physician preference, patient ability, equipment availability, and department protocol.
Attention to detail is crucial during the simulation process. A radiation therapist must review the physician’s order and accurately follow scan parameters and department protocol. Pre-simulation education is vital in preparing the patient for treatment. The patient will need a dental appointment before the simulation appointment to address dental caries and tooth extractions. If tooth extractions are indicated, it is recommended that radiation begins after a 2–3-week healing time, beginning treatments earlier can compromise wound healing. When scheduling the simulation, therapists should confirm that a dental appointment has been scheduled. Patients may also need to be informed if shaving is required before mask formation.
When the patient arrives, it is important to consider the beam angles required for treatment before constructing the immobilization device. Then, help the patient lie supine and straighten them on the table; use external landmarks such as the glabellum, SSN (suprasternal notch T2/3), and xiphoid (T9/10). Typically, patients are headfirst, with a thermoplastic head and shoulder mask, knee bolster, feet banded, and hands clasped together or holding a ring. However, every patient and clinic protocol is different. Some patients may present with unique challenges when it comes to positioning. Before fabricating an immobilization device, ensure that the patient is comfortable and in a reproducible position.

Thermoplastic masks play a significant role in reducing setup errors of head and neck treatments. A headrest is used to hyper-extend the patient’s chin so that the mandibular line to the mastoid tip is perpendicular to the table; this opens the cervical lymphatics and reduces the mandible dose. Before forming the thermoplastic mask, shoulder retraction may be indicated to help exclude the shoulders from interfering with the treatment path. Lastly, apply radiopaque markers (bb’s) at the lasers reference isocenter laterally on each side of the mask and anteriorly before the topogram. For inferiorly located treatments, an alignment mark at the inferior aspect of the mask and on the patient’s skin can help ensure the patient is straight. Localization marks should be near the center of the field and in a stable location, not near the edge of the shoulders. Most clinics mark the mask using a sharpie on tape to indicate the triangulation points.
Thorough documentation is essential for treatments of the head and neck due to the mobility of the structures and the numerous adjacent tissues with varying radiosensitivities. Photos, setup notes, and immobilization devices should be entered into the patient’s chart.
Special Simulation Considerations: H&N
Special considerations must be accounted for based on each patient’s unique needs and circumstances. For example, some people are claustrophobic and may need premedication before their simulation/treatment. Cutting the eyes out of the thermoplastic mask, using an open-faced mask, and playing music could all help calm a patient needing extra support. Patients with a previous medical history of limb weakness may need a strap to hold their arms. Additionally, patients with spinal conditions such as kyphosis or scoliosis may need a custom headrest to make them more comfortable. Radiation therapists can provide referrals for additional support services such as social work, cancer support groups, and music therapy. They should communicate the patient’s needs with the entire radiation oncology team.
Head and neck patients must remove any jewelry, hearing aids, or dentures before their simulation/treatment to ensure reproducibility and proper treatment delivery. A patient’s tumor location may also require a tongue depressor or bite plate placed in the patient’s mouth while the thermoplastic mask is formed. The purpose of the bite plate is to separate the tongue from the hard palate; this helps to exclude part of the tongue and oral mucosa, which is highly radiosensitive, from the treatment beams. This type of accessory plays a role in treating nasopharyngeal and oropharyngeal treatments. Additionally, patients with metal fillings could experience an increased mucosal reaction due to scatter; fluoride trays can help reduce the scatter. These trays should be worn for simulation and treatment and should have been made at the patient’s dental appointment.
Head and neck tumors are typically treated with lower energy (6X) beams. Higher energies have greater penetration which can miss superficial structures like the submental, sub digastric, and cervical lymph nodes. Higher energies are also a disadvantage due to the separation, radiosensitivity, and surrounding organs at risk.
Due to the many critical structures within the head and neck, a cone beam CT is performed before treatment delivery to ensure all necessary structures are included in the target volume. Different institutions and physicians may have unique preferences on what anatomical structures to align patient images; this should be documented in the patient’s chart.
|
Organ
|
Whole Organ Dose
|
Endpoint
|
|
Parotid
|
32 Gy
|
|
|
Spinal Cord
|
45 Gy
|
Myelitis/Necrosis
|
|
Tempo-mandibular Joint
|
60 Gy
|
Limitation of Joint Function
|
|
Larynx Cartilage
|
70 Gy
|
Necrosis
|
|
Larynx Vocal Cord
|
45 Gy
|
Edema
|
|
Thyroid
|
45 Gy
|
Thyroiditis
|
|
Lens
|
10 Gy
|
Cataracts
|
|
Lacrimal Gland
|
26 Gy
|
Dry Eye
|
|
Optic Chiasm
|
50 Gy
|
Blindness
|
|
Optic Nerve
|
50 Gy
|
Blindness
|
|
Brain (Temporal Lobe)
|
47 Gy
|
Necrosis/Infarction
|
|
Brainstem
|
50 Gy
|
Necrosis/Infarction
|
|
Ear
|
55 Gy
|
Chronic Serous Otitis
|
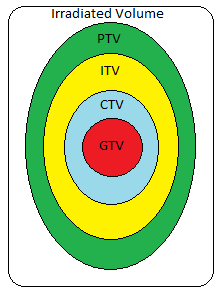
The general treatment margins for head and neck cancers includes a 5 mm PTV expansion of the gross disease (GTV), which will receive the highest dose. The elective treatment areas, the lymph nodes at risk for microscopic disease, perineural pathways, and the anatomical compartment have a 3 mm expansion. The expansion may change depending on the surrounding adjacent structures. These margins are much tighter than what was used with conventional treatment. With recent advancements in treatment localization and modern imaging techniques combined with proper immobilization, providers can have confidence in the reproducibility and consistency of these increasingly shrinking margins.
|
Gross Tumor Volume (GTV)
|
The gross demonstrable extent and location of disease that can be seen or felt.
|
|
Clinical Target Volume (CTV)
|
Includes the GTV plus a margin to account for microscopic disease that cannot be seen or felt. The area outside the CTV is presumed to have no cancer cells.
|
|
Internal Target Volume (ITV)
|
Accounts for internal motion (breathing, peristalsis, bladder filling, etc.). GTV plus margin for motion = ITV.
|
|
Planning Target Volume (PTV)
|
Includes the CTV plus a margin to account for possible geometric uncertainties, such as patient set-up.
|
|
Treatment Volume (TV)
|
Volume covered by the prescription isodose line. Volume is determined by delivery technique.
|
|
Irradiated Volume
|
Volume that receives a significant dose, usually defined as 50% of prescription dose. Volume is determined by delivery technique.
|
|
Organ at Risk Volume (OAR)
|
Volume encompassing a normal tissue whose radiation sensitivity may significantly influence treatment planning. Example: lens of eye, salivary glands, spinal cord, etc.
|
Squamous cell carcinoma of the head and neck are treated to approximately 70 Gy. The general curative dose-fractionation for head and neck cancers is 45-50 Gy to elective treatment regions and 60-70 Gy to the gross disease in 30-35 fractions, with a daily fractionation of 1.8-2 Gy.
Other fractionation schemes used in head and neck treatments include:
- Twice daily (bid): Hyper fractionated treatments deliver a smaller dose per fraction for the same number of treatment days and weeks as conventional fractionation. There is a 6-hour minimum between treatments for the reassortment, repair, repopulation of normal cells, and reoxygenation of the tissues.
- Quad shot: Hypo fractionated treatment used in patients with head and neck carcinoma. Palliative radiation therapy is delivered bid. on two consecutive days (4 fractions) to 14-14.8 Gy. Patients can receive up to three cycles at 4-week intervals.
Treatment Techniques: H&N
The disease site, function, and cosmesis strongly influence surgical options for head and neck cancers. Surgical resection may be challenging because of the surrounding critical structures. For example, most nasopharyngeal diagnoses, surgery is not possible due to anatomic constraints but is reserved as a salvage option. A radical nasopharyngectomy and a neck dissection may be indicated for residual or recurrent disease. Surgery can be performed as the initial or primary treatment for small lesions or after neoadjuvant chemotherapy or radiation.
Adjuvant chemotherapy is used with radiation as a radiosensitizer, which enhances the lethal effects of radiation therapy. This may be the case for advanced-stage tumors that are unresectable, post-operative, and for patients with positive surgical margins or extranodal extension. Chemotherapy can lead to a significant improvement in survival and locoregional control compared to giving radiation alone. Cisplatin is a common chemotherapy agent used for head and neck malignancies.
Intensity Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) have become the standard radiation therapy treatment technique for head and neck cancer. These treatment techniques can achieve a more conformal plan to complex target volumes. IMRT and VMAT are the preferred treatment modalities because the local extent of the disease is better encompassed while sparing healthy tissues and organs at risk.
Conventional treatments are used to treat midline lesions and bilateral neck node involvement cases with opposed lateral fields, which does not allow the sparing of the adjacent mucosa. For one-sided lesions, anterior and posterior oblique wedged fields were implemented with a lateral field to improve dose homogeneity.
Electrons are a treatment option for superficial structures like the lip, parotid, or lymph nodes. If electrons are used, it is crucial to ensure the cone is placed en face to the involved area. Ensure that the treatment beam is perpendicular to the patient’s surface and the electron block is parallel to the skin surface to achieve a proper dose distribution.
Brachytherapy is typically utilized for recurrence or as a boost after chemoradiation. Brachytherapy can be used through an intraoral cone or interstitial implant for small cancers, not close to the bone and accessible for implantation. Although brachytherapy is rarely performed, it offers the advantage of sparing normal tissues.
|
Side Effect
|
Dose
|
Treatment
|
|
Decreased saliva
Loss of salivary function |
20 Gy
40-45 Gy |
Olive oil, ice chips, sugar free gum or candy, Biotene or other over the counter products, etc.
|
|
Skin reactions:
Faint erythema
Erythema Dry desquamation Moist desquamation |
16 Gy
20-30 Gy 30-40 Gy 40-60 Gy |
Assess skin integrity, apply recommended moisturizing lotions free from alcohols or perfumes, avoid drastic temperatures, wear loose cotton clothing, avoid razor shaving, aerate skin folds, if dry and/or moist desquamation occurs may need prescription creams or other interventions
|
|
Tumoritis
|
20 Gy
|
Redness of the tumor; helps define tumor extent
|
|
Mucositis/stomatitis
|
30 Gy
|
Soft bland, and moderate temperature diet
|
|
Dysphagia, pharyngitis, odynophagia, esophagitis
|
20-30 Gy
|
Saline gargle; soft bland, and moderate temperature diet
|
|
Taste alterations
|
10 Gy
|
Seasoning, sugar, marinating, chew thoroughly
|
|
Trismus
|
60 Gy
|
Exercise muscles, change diet, surgery
|
|
Dental caries
|
50-60 Gy
|
Extract diseased teeth
|
|
Fatigue
|
10 Gy
|
Rest and fluids
|
Emerging Technologies & Treatments: Head & Neck
Advances in technology are happening more rapidly than ever before. Today, several treatment technologies and devices have increased the accuracy and reduced treatment time for head and neck malignancies. A few treatment advancements include:
- 6 degrees of freedom tables – Correct for patient tilt and rotation issues (Vendor examples: Protura & Hexapod)
- Infrared motion/surface monitoring systems (Vendor examples: AlignRT)
- Proton beam radiation therapy is another treatment modality that can be used to treat the head and neck. Protons only travel a certain distance, so the tissues behind the cancer are exposed to very little radiation. Even the tissues in front of the tumor see less radiation than the tumor itself. Therefore, protons deliver radiation to cancer while minimizing damage to nearby healthy tissues.
- Targeted therapy uses drugs to target specific genes and proteins that enable cancerous cells to survive and grow. The downside to this emerging technology is that not all hospitals and clinics offer targeted therapy to patients because it is a growing treatment technique still being researched and studied. Target therapies continue to be investigated for their use in treating head and neck cancers.
- Immunotherapy is another emerging technology that is also called biologic therapy. Immunotherapy works by increasing the body’s defense mechanisms to fight cancer. The role of immunotherapy in metastatic head and neck squamous cell carcinoma is evolving.
- Photodynamic therapy uses a photosensitive substance, which is a substance that is sensitive to light, to allow for tumor localization. This photosensitive substance is injected into the patient’s bloodstream, and the cancerous cells that are present then harbor it and hold onto the substance longer than the healthy cells. Lasers are then directed at the tumor, which activates the substance to destroy the cancerous cells.
- Neutron therapy (Boron Neutron Capture Therapy – BNCT) is a technique that is being used for unresectable salivary gland cancers and other difficult to treat cancers. Studies show that treatments with neutrons, instead of conventional x-rays or electrons, can increase the local control rate and reduce the risk of late toxicity.
Media Attributions
- Anatomical divisions and major structures of the head and neck © Jared Stiles adapted by Jared Stiles is licensed under a CC BY (Attribution) license
- Cervical lymph nodes and levels © Mikael Häggström, M.D. is licensed under a CC0 (Creative Commons Zero) license
- Diagram showing the position of a percutaneous endoscopic gastrostomy (PEG) feeding tube © Cancer Research UK is licensed under a CC BY-SA (Attribution ShareAlike) license
- Chevallet fracture -x-ray lateral view of skull and neck © https://en.wikipedia.org/wiki/User:Sbks_medicos adapted by Jared Stiles is licensed under a CC0 (Creative Commons Zero) license
- S-Frame Variable Perf™ Head & Shoulder © CQ Medical is licensed under a All Rights Reserved license
- Planning target volumes © Jared Stiles is licensed under a CC BY (Attribution) license
Treatment given after the initial treatment of cancer to remove remaining cancer cells or to prevent recurrence
both sides
The physical signs and symptoms of a disease that doctors use to assess and diagnose a patient's condition
Refers to the other side (of the body)
An older technique that uses 2D x-ray imaging during the planning process and a small number (2-4) of square fields for treatment
Maintaining or restoring a pleasing or natural physical appearance
The time it takes for a tumor to double in size
The radiation is perpendicular to the skin surface.
Surgical removal of one half of the tongue
fewer fractions at a higher dose
Refers to the same side (of the body)
Surgical removal of the lymph nodes and surrounding tissue in the neck
The treatment given before the main cancer treatment
Percutaneous endoscopic gastrostomy (PEG) where a feeding tube is placed through the abdomen into the stomach
The redistribution of cells over different cell cycles after each fraction
Lymph nodes in proximity to the primary tumor
A device used to press the tongue down
dry mouth
The anterior lower neck field of the 3-field technique called "yoke" because its field shape looks like the yoke on a pair of oxen


