29 Overview: Lymphoma
- Describe the anatomy, structures, and landmarks of the lymphomas
- Describe the differences between the types of lymphomas
- Describe the simulation process for lymphomas
- Identify commonly used positioning & immobilization devices used
- Define scan parameters and reference isocenter location for simulation
- Discuss special considerations in patient positioning
- Define treatment borders and how they relate to tumor spread
- Describe tumor volumes and margins
- Discuss the treatment procedure for lymphomas
- Perform tasks associated with the simulation and treatment of lymphoma patients
Key Terms
Overview: Lymphoma
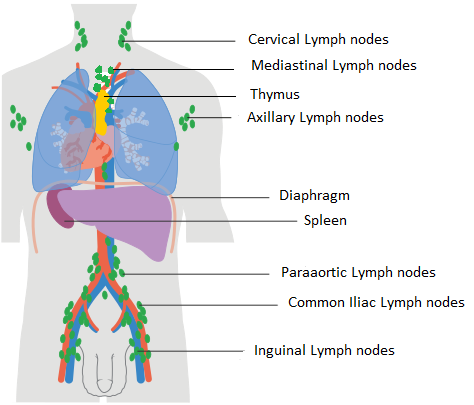
Lymphomas are a classification of blood cancers affecting the body’s lymphocytes, a type of white blood cell that is responsible for immunity. The disease most commonly affects the lymph nodes and spleen but can be found in lymphatic tissues that exist throughout the body. For example, MALT (mucosa-associated lymphoid tissue) lymphoma originates in tissues of the lungs, stomach, intestines, or salivary glands; these tissues help in immunity.
Lymphomas are the most common malignancy in adolescents ages 15-19. The exact cause of lymphoma is not well understood, but it is associated with factors such as genetics, viral infections (e.g., Epstein-Barr virus), exposure to certain chemicals, and radiation. Common symptoms of lymphoma may include enlarged lymph nodes, fatigue, itching, and B-symptoms. If B-symptoms are present, it may indicate a more advanced and aggressive disease.
The primary treatment option for lymphomas is chemotherapy, but other options include radiation therapy, immunotherapy, targeted therapies, and stem cell transplantation. Radiation therapy continues to have an important role in the locoregional control of the disease and improving overall outcomes, especially for patients with residual or refractory disease. The treatment depends on the type, stage, and the individual patient’s needs. Lymphomas are typically of B-cell origin and are broadly categorized into two main types, Hodgkin lymphoma and non-Hodgkin lymphoma (NHL), although several other subtypes exist.
- Hodgkin lymphoma is characterized by the presence of Reed-Sternberg cells. The spread of these cancers is predictable following the lymphatic drainage pathways and has a relatively high cure rate (~90%). Subtypes include Nodular sclerosing (70%), Mixed cellularity, Lymphocyte rich, and Lymphocyte depleted.
- Non-Hodgkin lymphoma (NHL) is more common than Hodgkin lymphoma. It can develop in both children and adults and has a wide range of characteristics and treatment options. The spread of NHL is not predictable. Some common subtypes include Diffuse large B-cell, Follicular, Mantle Cell, Burkitt, and Hairy Cell, and T-cell. Cutaneous lymphomas are a lymphoma of the skin – mycosis fungoides is the most common. Cutaneous lymphomas may require TSEI (total skin electron irradiation).
The prognosis for patients with Hodgkin’s is largely determined by the stage at diagnosis and initial management. Failure to control the disease in the first round of treatment often constitutes a life-threatening situation for the patient. Disease progression often necessitates more aggressive interventions, such as salvage chemotherapy or stem cell transplants, which carry higher risks and side effects, making it crucial to aim for effective initial disease control.
Learn more about Lymphomas through The American Cancer Society.
Patient Simulation: Lymphoma
The simulation process for lymphoma is site dependent. For disease above the diaphragm, in the head and neck area, patients are simulated supine with a head and shoulder mask, arms akimbo, and a knee bolster. For mediastinal disease, patients can be positioned supine with their arms above their head in an arm-board or vaclok. Scanning parameters may include the vertex through the second lumber vertebra.
For treatments below the diaphragm, patients are positioned supine with a pillow under their head, arms at their side or high on their chest, with a vaclok under their legs. Scan parameters extend from the carina through the pelvis.
Patients with disease on both sides of the diaphragm receiving total lymph node irradiation will use a combination of immobilization for their upper and lower body. Their arms should be placed at their sides with arms akimbo. Scan parameters extend from vertex through the pelvis.

Special Simulation Considerations: Lymphoma
For disease above the diaphragm, a headrest that elevates the chin will allow the submental, submandibular, and cervical lymph nodes to be treated while excluding the mandible and oral cavity. If the axillary nodes are included in the treatment, positioning the patient’s arms above their head or akimbo helps reduce the skin folds in the axilla and reduces the skin reaction. If the patient’s arms are above their head, humeral head reproducibility is important. If the arms position is too high, compared the simulation position, the axillary nodes may be inadvertently blocked. If the arm position is too low, the humeral head could be included in the radiation field. Young female patients may benefit from moving or taping the breast tissue away from the radiation field.
For disease below the diaphragm, an oophoropexy may be performed to relocate the ovaries out of the radiation field to preserve fertility. For males receiving treatment with inverted-Y fields, they may benefit from the use of a testicular shield to reduce the internal scatter received. Treatment areas close to the diaphragm may exhibit excessive motion. Gating or a breath-hold technique may be employed to reduce the volume of normal tissue irradiation.
Treatment Volume Localization: Lymphoma
For stage I & II lymphoma, disease is confined to one side of the diaphragm. For Stage III or IV, disease is found on both sides of the diaphragm. The CTV can be determined through pretreatment imaging – this entire volume, in most situations, should be included in the treatment field. If pretreatment imaging is unavailable, information obtained through a simulation PET/CT and MRI will be valuable in the treatment plan design.
If the treatment site has respiratory motion, an expansion of 1-2 cm may be necessary – this volume is termed the ITV (internal target volume). The PTV (prescribed treatment volume) accounts for the CTV/ITV and any setup uncertainties during treatment and varies by institution and physician. The spleen may be included in the treatment field if positive for disease. If included, the dose to the kidneys should be closely monitored.
Organs at risk are subject to the involved site’s location. Above the diaphragm, the lungs, heart, cord, and esophagus are structures of most concern. Below the diaphragm, the liver, kidneys, small bowel, colon, and ovaries are of concern.
Treatment Techniques: Lymphoma
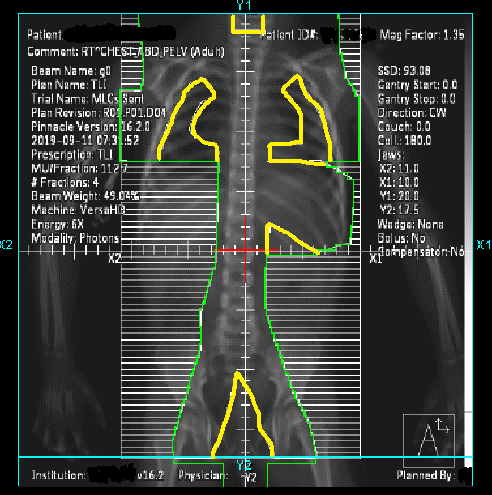
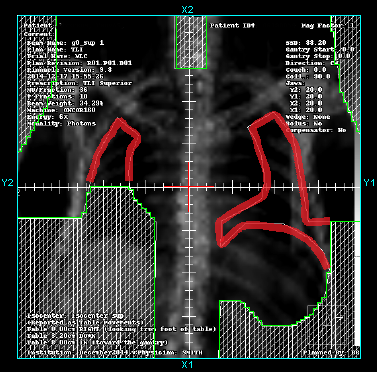
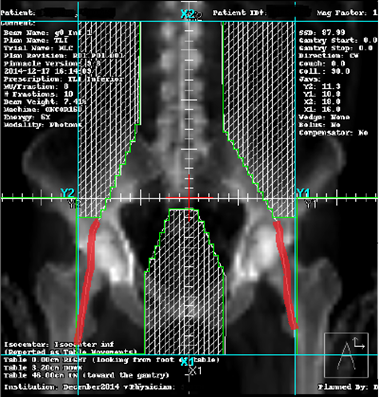
If disease is on both sides of the diaphragm, total nodal irradiation may be required. The field above the diaphragm was historically termed the mantle-field. The field includes the major lymphatics above the diaphragm and blocks the normal lung tissue, larynx, and humeral heads. Below the diaphragm, the field was termed the inverted-Y and comprised of a pelvic and a paraaortic portion.
The mantle and inverted-Y fields are an “extended-field” technique. The treatment fields match about the tenth vertebral level. The treatment plan must prevent beam overlap using a match line or feathering technique technique.

Lymphomas are radiosensitive and respond well to lower treatment doses. The total dose delivered will depend on the patient’s histology subtype and clinical risk factors. Generally, treatment doses are 20-30 Gy for favorable disease or 30-40 Gy for relapsed disease or patients with unfavorable characteristics.
Treatment technique selection will depend on the disease location. Historically, patients were treated with an AP/PA technique. Treatment fields today are reduced to areas of known disease termed an “involved field” technique. Conformal 3D-fields are common practice today. AP/PA treatment fields offer a reduced irradiated volume, but IMRT or VMAT may be desired for better sparing of critical structures.
Emerging Technologies & Treatments: Lymphoma
More recent techniques focus on the “involved site” and “involved node” radiation therapy and further reducing normal tissue exposure. The application of proton therapy continues to be investigated.
Media Attributions
- Lymph node diagram © Cancer Research UK; Wikimedia Commons adapted by Jared Stiles is licensed under a CC BY-SA (Attribution ShareAlike) license
- arms akimbo © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Total nodal irradiation © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- upper total nodal © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- TNI lung photon block © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- lower total nodal © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
Arms bent with hands on the hips
include fever, night sweats, and unintentional weight loss of 10% over six months
a systemic type of cancer treatment that uses drugs to destroy cancer cells or inhibit their growth and division
using the MLCs to "blend" the dose at a field junction and reduce the likelihood of a hot or cold spot.
a type of cancer treatment that uses the body's own immune system to recognize and fight cancer cells
surgical procedure in which one or both ovaries are relocated and secured to a different position within the body to protect them from damage during radiation therapy
large, abnormal cells that are characteristic of Hodgkin lymphoma
cancer that remains or is resistant to treatment
designed to interfere with particular molecules involved in tumor growth, survival, and spread
top of head

