23 Overview: Pelvis
- Describe the anatomy, structures, and landmarks of the male and female pelvis
- Describe the malignancies of the pelvis
- Describe the simulation process
- Identify commonly used positioning & immobilization devices used for pelvis treatments
- Define scan parameters and reference isocenter location for pelvis simulations
- Discuss special considerations in cancers of the pelvis
- Define treatment borders and how they relate to tumor spread in the pelvis
- Describe tumor volumes and margins of cancers of the pelvis
- Discuss the various treatment procedures of pelvic malignancies
- Perform tasks associated with the simulation and treatment of pelvic malignancies
Key Terms
Overview: Pelvis
Cancers of the pelvis that affect both males and females include cancers of the lower gastrointestinal tract including the colon, rectum, and anus and those of the urinary system including the ureters, bladder, and urethra. Rectal cancer is commonly grouped with cancers of colon in terms of epidemiology and are often referred to as colorectal cancers. Colorectal cancers are the 3rd most common malignancy in the US with males having slightly higher incidence rates over females. A screening colonoscopy examines the colon and rectum for polyps or signs of cancer and is recommended for those of average risk beginning at age 45.
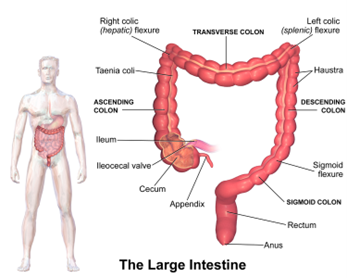
The colon begins with the cecum in the lower right of the pelvis where the small intestine’s ileum terminates. From the cecum, the colon then ascends superiorly (ascending colon) to the hepatic flexure near the liver, then travels horizontally from right to left (transverse colon), turning close to the level of the spleen (splenic flexure), and then descends inferiorly down the left side (descending colon). It then makes an S-shaped curve called the sigmoid colon as it moves back into the pelvis and more midline. From there it proceeds inferiorly into the rectum, and eventually the anus as it exits the body.
The dentate line separates the rectum and anus. The transition from glandular tissue of the rectum and squamous cell tissues of the anus occurs here. Most colon and rectal cancers are adenocarcinomas and anal cancers are typically squamous cell carcinomas. Anal cancer is twice as common in women than men. Rectal or anal bleeding or change in bowel habits are common presenting signs of colorectal or anal cancers.
Risk factors for colorectal cancer include high fat, low fiber diets, smoking, alcohol use, inflammatory bowel disease, and genetic predisposition. Common routes of spread include invasion of adjacent pelvis structures and lymphatic spread to the mesenteric, peri-rectal, internal iliac, and sacral lymph nodes. Risk factors for anal cancer include HPV, HIV, smoking, and anal intercourse. The common route of spread is drainage to the inguinal lymph nodes .Cancers of the urinary system are more common in males; most cancers occur from transitional (urothelial) epithelium cells. Bladder cancer is the most common urinary malignancy and is typically diagnosed in the 50–60 year-old population. Patients usually present with gross hematuria at the time of diagnosis.
Risk factors for bladder cancer include cigarette smoking, chronic bladder irritation, and exposure to aniline dyes. The triangular area between the three orifices (ureter and two urethra) is termed the trigone; this area is one of the most common sites for carcinoma. Common routes of spread for bladder cancer are through direct extension and the bladder wall. More specific information about male and female pelvic cancers is listed below.
A general overview and explanation for the common screening types of cancers of the pelvis can be found in the link below. Please see individual sections for specific cancer screening types.
Cancer Screening Guidelines | Detecting Cancer Early
An essential part of the patient’s treatment plan is the simulation process. The simulation is performed after the patient has met with the doctor and consented to radiation therapy treatments. The physician completes an image request for simulation specifying positioning and treatment considerations. This should include the patient’s specific treatment site, contrast orders for the CT simulation, positioning, type of immobilization devices, and scan parameters. Standards and similarities exist across the profession, but differences could occur due to physician preference, patient ability, equipment availability, and department protocol.
Attention to detail is crucial during the simulation process. Reviewing the physician’s order and accurately following scan parameters is an essential role of a radiation therapist. Considering the beam angles required for treatment before constructing the immobilization device is vital. Begin by helping the patient lie on the table and straighten them using the overhead sagittal laser aligning to the patient’s midline. Many pelvis patients are positioned supine. However, there are some cases where prone is a better option for the treatment plan and are discussed in “Special Simulation Considerations.” Typically, patients are headfirst, with pillows under the head and an immobilization device called a vaclok under their legs. As always, before fabricating an immobilization device, ensure that the patient is in a reproducible position and is as comfortable as possible and able tolerate the position for the anticipated length of treatment.
Detailed documentation of the simulation procedure is necessary, as different therapists will likely perform the patient’s verification setup and treatments. Include photos, setup notes, and immobilization devices in the patient’s chart or record and verify system. This is especially important for pelvic cancers because there are often special instructions for the bladder fullness and rectal emptying. A full bladder scan and an empty bladder scan may be acquired to determine the internal target volume and account for variability that could occur during the treatment course. Intravenous contrast and oral contrast may be used for better delineation of the contrast-enhanced pelvic vessels and bowel contouring. The therapist should ask the patient each day if their bladder is full or empty as instructed before treatment and verify with imaging.
Special Simulation Considerations: Pelvis
Each patient’s unique needs and disease circumstances may require changes to their simulation setup. For example, educating patients on the importance of their position enhances their understanding and cooperation to hold still during treatment. When treating the pelvis, the patient is typically positioned supine or prone.
Supine Position: Patients are often positioned in a supine position when treating the pelvis as it is a more stable and tolerable position. Another benefit of this position is the ability to visualize the inguinal nodal areas commonly included in the treatment volume. Positioning and immobilization devices include pillows under the head, a low extremity to reproduce the hips and pelvic position, and/or a knee bolster. For patients requiring the inclusion of inguinal nodes in the treatment fields, positioning their legs in a frog-leg or spread-out knee position helps with better visualization of the inguinal nodes and reduces skin folds that could lead to more severe skin reactions during the course of treatment. The arms are typically placed high on the patient’s chest or above the head if treating para-aortic nodes to keep them out of the treatment field.

Prone Position: The prone position is another treatment setup commonly used for treatments of the pelvis – primarily rectal cancers. The main advantage of prone positioning is the small bowel falls forward out of the pelvis, reducing its dose. Most patients benefit from the prone position, regardless of size, however, patients with a strong abdominal muscle tone may not benefit as much. The position also allows the glutes to fall apart, resulting in less skin-on-skin contact, helping reduce scatter and skin reactions. A belly-board or custom prone vaclok device with an anterior void allows allows the radiosensitive small bowel to fall anteriorly out of the pelvis. The patient is indexed longitudinally on the belly-board using a ruler found on the right and left lateral sides of the board – this will help achieve a consistent pelvic tilt throughout the course of treatment. The pubic symphysis should sit at the inferior ridge of the belly board to displace as much small bowel as possible.

Physicians often instruct pelvic patients to have a comfortably full bladder for simulation and throughout treatment to enhance reproducibility internally and reduce dose to surrounding structures. A comfortably full bladder will push the small bowel superior out of the treatment fields. However, when treating the bladder, patients are coached to have an empty bladder to reduce the size of the treatment field. During simulation, it is also critical to monitor the fullness of the rectum. An empty rectum will prevent the bowel from pushing on adjacent structures into the treatment field. Depending on the doctor’s preference, external radiopaque markers may be placed on the anal or vaginal verge to visualize and ensure adequate tumor coverage.
Contrast may be administered during simulation to enhance critical structures in the treatment area. Male urethral contrast may be inserted and held in place by a penile clamp. Intravenous contrast may be used to better visualize the bladder, lymph nodes, and vessels. Oral contrast may also be necessary to visualize the small bowel.
Tumors of the pelvis are typically treated with higher energy beams (10MV to 18MV) due to tumor depth and subsequent beam attenuation. IMRT and VMAT techniques are currently not possible with 18 MV beams, treatments at this energy use static fields.
|
Organ at Risk (OARs)
|
TD 5/5 Whole Organ
|
Outcome Associated
|
|
Bladder
|
65 Gy
|
Bladder contracture/Volume loss
|
|
Rectum
|
60 Gy
|
Proctitis/Necrosis/Fistula
|
|
Small Bowel
|
45 Gy
|
Obstruction/Perforation/Fistula
|
|
Large Bowel
|
50 Gy
|
Obstruction/Perforation/Ulceration/Fistula
|
|
Femoral heads
|
52 Gy
|
Necrosis
|
|
Spinal Cord
|
45 Gy
|
Myelitis/Necrosis
|
Treatment Margins:
At the University of Iowa Hospitals, treatment margins are organized by grouping all gynecological sites together and isolating the prostate separately. The treatment techniques used are specific for each group. For instance, limiting the rectal dose when treating the prostate is of great concern, whereas considering the clinical spread of the disease is more critical for gynecological cancers.
The standard practice for treating the prostate margins is to encompasses the prostate and seminal vesicles with a 6 mm expansion in all directions except posteriorly. Posteriorly the expansion is limited to 4 mm due to the rectum’s proximity. These margins are for standard fractionation on a linear accelerator. Treatment units with ATS (adapt-to-shape) capabilities allow for tighter margins of 5 mm in all directions with a 3 mm posterior margin.
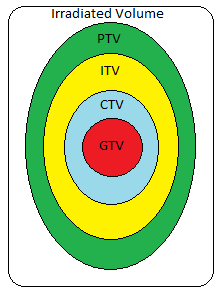
Regarding gynecological margins, the rule of thumb is an expansion from the involved nodes. GTVs and CTVs will not expand into bone due to the much lower likelihood of the disease spreading to the bone than involved tissues. There will commonly be a 7 mm margin around the GTVs of solid tumors with a 5 mm expansion to create the CTV to PTV margins. The increased PTV considers the inherent inconsistencies with daily setup reproducibility.
|
Gross Tumor Volume (GTV)
|
The gross demonstrable extent and location of disease that can be seen or felt
|
|
Clinical Target Volume (CTV)
|
Includes the GTV plus a margin to account for microscopic disease that cannot be seen or felt
|
|
Internal Target Volume (ITV)
|
Includes the CTV plus a margin to account for internal motion of the target
|
|
Planning Target Volume (PTV)
|
Includes the CTV and ITV plus a margin to account for possible geometric uncertainties, such as patient set-up
|
|
Treatment Volume (TV)
|
Volume covered by the prescription isodose line
|
|
Irradiated Volume
|
Volume that receives a significant dose, usually defined as 50% of prescription dose
|
|
Organ at Risk Volume (OAR)
|
Volume encompassing a normal tissue whose radiation sensitivity may significantly influence treatment planning
|
Traditional field borders of the pelvis remain consistent laterally with a 1-2 cm margin beyond the pelvis inlet to include the common iliac nodes. The next chapters include site-specific borders and describe the superior, inferior, anterior, and posterior treatment margins.
The general curative dose-fractionation for pelvic cancers is 45-50 Gy followed by a boost. The PTV includes the tumor volume and regional lymph nodes. A boost to the GTV and involved areas follows with a daily fractionation of 1.8 to 2 Gy. The total dose is dependent on the primary site and organs at risk; these are are described in future site-specific chapters.
The treatment plan chosen for a patient is based on several different factors. These factors include the sites of possible regional involvement, the performance status of the patient (Karnofsky Performance Scale/KPS), and the extension of the primary disease.
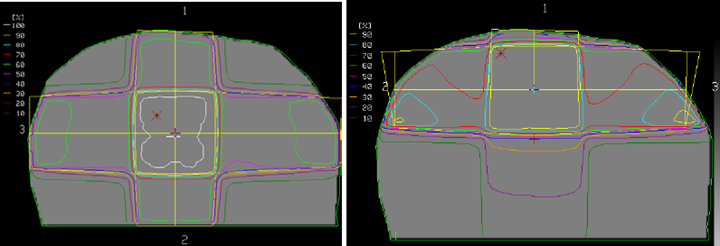
Three-dimensional conformal treatment techniques commonly used in treating the pelvis are three and four-field beam arrangements.
- The three-field treatment includes a posteroanterior (PA) field and opposed lateral fields with wedges. The heel of the wedges is placed posteriorly, where the PA and lateral beams meet, to reduce hotspots in the posterior pelvis. The three-field technique is most seen for patients positioned prone when treating rectal cancer.
- A four-field treatment, “box” technique, the beam arrangement is AP/PA and opposed lateral fields. This method is used when anterior structures like the prostate or vagina are involved or at risk for disease. When treating a four-field pelvis, it is preferred to use higher energies to fully penetrate to the deep pelvis and reduce hotspots in the more superficial tissues of the pelvis. Sometimes beams are weighted more posterior or anteriorly depending on the structures involved. For example, if treating the rectum, the posterior beam may deliver a higher dose.
Intensity Modulated Radiation Therapy (IMRT)/Volumetric Modulated Arc Therapy (VMAT) have become the standard radiation therapy treatment technique for pelvic cancer, allowing for more sparing of the small bowel, colon, bladder, and femoral heads.
Brachytherapy is another treatment modality frequently used in treatments of the pelvis. The technique is a form of internal radiation therapy that uses sealed radiation sources. The sources are placed inside the patient’s body beside or within the tumor. This treatment delivery technique spares the surrounding healthy tissues and improves survival outcomes. Brachytherapy is commonly prescribed for prostate, endometrial, cervical, and vaginal cancers.
Emerging Technologies & Treatments: Pelvis
Advances in technology are happening more rapidly than ever before. Today, several treatment technologies and devices have increased treatment accuracy and reduced treatment time for pelvis malignancies. A few treatment advancements include:
- 6 degrees of freedom tables – Corrections for patient tilt and rotation (Vendor examples: Protura & Hexapod).
- Infrared motion/surface monitoring systems (Vendor example: AlignRT)
- Proton beam radiation therapy is another treatment modality that can be used to treat the pelvis. Protons have unique physical properties and only travel a certain distance based on their energy. By adjusting the energy, the depth the dose is deposited is controlled which means treatments are delivered using only one or two lateral beams. The tissues before (entrance dose) and after (exit dose) the cancer receive minimal radiation, reducing side effects.
- ART – Adaptive Radiation Therapy is an advanced treatment technique that optimizes patients’ treatment plans daily based on real-time imaging with MRI or CT scans. This technique ensures the radiation is delivered precisely to the tumor while minimizing damage to healthy tissues. By adapting the treatment to the patient’s changing anatomy and tumor characteristics, ART increases treatment accuracy and efficacy, potentially improving patient outcomes and reducing side effects. (Vendor examples: Varian Ethos, Elekta Unity, ViewRay, MRIdian)
Media Attributions
- The Large Intestine © BruceBlaus is licensed under a CC BY (Attribution) license
- supine pelvis © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- prone pelvis © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Pelvis: Prone © Jared Stiles adapted by Jared Stiles is licensed under a CC BY (Attribution) license
- Pelvis: Bladder Fullness © Jared Stiles adapted by Jared Stiles is licensed under a CC BY (Attribution) license
- Planning target volumes © Jared Stiles is licensed under a CC BY (Attribution) license
- 4-field plan of the middle pelvis vs. a 3-field plan of the posterior pelvis © The University of Iowa Radiation Therapy Program is licensed under a CC BY (Attribution) license
- Pelvis: 3 v. 4-Field © Jared Stiles is licensed under a CC BY (Attribution) license
Hormone therapy for prostate cancer that reduces testosterone to prevent cancer cells from growing and spreading
From front (anterior) to back (posterior)
A test done by a doctor that examines the lower rectum, posterior wall of the prostate, and anus
A global organization combining professional societies of obstetricians and gynecologists
the amount of blood in the urine is high enough to be visible upon inspection
Positioning aids used to maintain and reproduce the patient's position for radiation treatment
Describes a woman who hasn't given birth to a child
Two radiation fields treating the left and right side
Refers to forming new bone or osteoblasts and are commonly seen in prostate cancer
A protein produced in the prostate
A hormone therapy drug used to treat hormone receptor-positive breast cancer
A triangular area at the base of the bladder between the ureters and urethra
A vaclok is a bean bag-like device that molds around the patient and holds its shape when air is removed with a vacuum




